Global Neonatal & Children's Health
Global Neonatal & Children's Health 1
624 - The Three Delays-in-Healthcare model applied to mortality among infants and children aged 1-59 months in seven high mortality regions
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 624
Publication Number: 624.315
Publication Number: 624.315
Elisa Garcia Gomez, Emory University School of Medicine, Atlanta, GA, United States; Zachary Madewell, CDC, Atlanta, GA, United States; Ariel Nhacolo, Centro de Investigacao em Saude de Manhica, Manhica, Maputo, Mozambique; Quique Bassat, ISGlobal, Barcelona, Catalonia, Spain; Ikechukwu Ogbuanu, Emory University School of Medicine, Leesburg, GA, United States; Portia Chipo. Mutevedzi, CHAMPS Emory university, Johannesburg, Gauteng, South Africa; Dianna Blau, Other, Atlanta, GA, United States; J. Anthony G. Scott, London School of Hygiene & Tropical Medicine, London, England, United Kingdom; Nega Assefa, Haramaya University, Harar, Hareri Hizb, Ethiopia; Lola Madrid, London School of Hygiene and Tropical Medicine, Harar, Hareri Hizb, Ethiopia; Stian MS. Orlien, University of Hargeisa, Oslo, Oslo, Norway; Adama Mamby. Keita, CVD-Mali, Bamako, Bamako, Mali; Ashka Mehta, University of Maryland School of Medicine, Baltimore, MD, United States; David Torres-Fernandez, ISGlobal, Barcelona, Catalonia, Spain; Shams E. Arifeen, International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), Dhaka, Dhaka, Bangladesh; Emily S. Gurley, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States; Mohammad Zahid. Hossain, INTERNATIONAL CENTRE FOR DIARRHOEAL DISEASE RESEARCH, BANGLADESH (icddr,b), Dhaka, Dhaka, Bangladesh; Atique Iqbal. Chowdhury, icddr,b, Dhaka, Dhaka, Bangladesh; Kazi Munisul. Islam, icddr,b, Dhaka, Dhaka, Bangladesh; Ziyaad Dangor, University of the Witwatersrand, Soweto, Gauteng, South Africa; Sana Mahtab, WITS health consortium - VIDA, Johannesburg, Gauteng, South Africa; Amy J. Wise, University of the Witwatersrand, Johannesburg, Gauteng, South Africa; Yasmin Adam, University of the Witwatersrand, Johannesburg, Gauteng, South Africa; Carrie Jo Cain, Child Health and Mortality Prevention Surveillance, Blaine, MN, United States; Cynthia G.. Whitney, Emory University, Atlanta, GA, United States; Beth A. Barr, Nyanja Health Research Institute, Leopard Bay, Salima, Malawi; Chris A. Rees, Emory University School of Medicine, ATLANTA, GA, United States

Elisa Garcia Gomez, BS (she/her/hers)
Medical Student
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Delays in healthcare seeking and the provision of appropriate clinical care for infants and children are common in resource-limited settings. However, the contribution of such delays to persistently high childhood mortality rates is unclear.
Objective: Our objective was to describe delays in healthcare seeking among caregivers of, and healthcare provision for, deceased infants and children using the “Three Delays-in-Healthcare” model as a framework.
Design/Methods: We conducted a retrospective, descriptive study using data collected on infants and children aged 1-59 months who died between December 2016 and February 2022 in six sites in sub-Saharan Africa and one in Bangladesh and enrolled in the Child Health and Mortality Prevention Surveillance (CHAMPS) Network. We reviewed narratives provided by caregivers of deceased infants and children collected using the 2016 WHO Verbal Autopsy form and clinical summaries extracted from medical charts. Delays in 1) illness recognition in the home/decision to seek care, 2) transportation to healthcare facilities, and 3) the provision of adequate clinical care were extracted from summaries and categorized according to the “Three Delays-in-Healthcare” model. Comparisons in each delay by age and site were made using Chi-square testing.
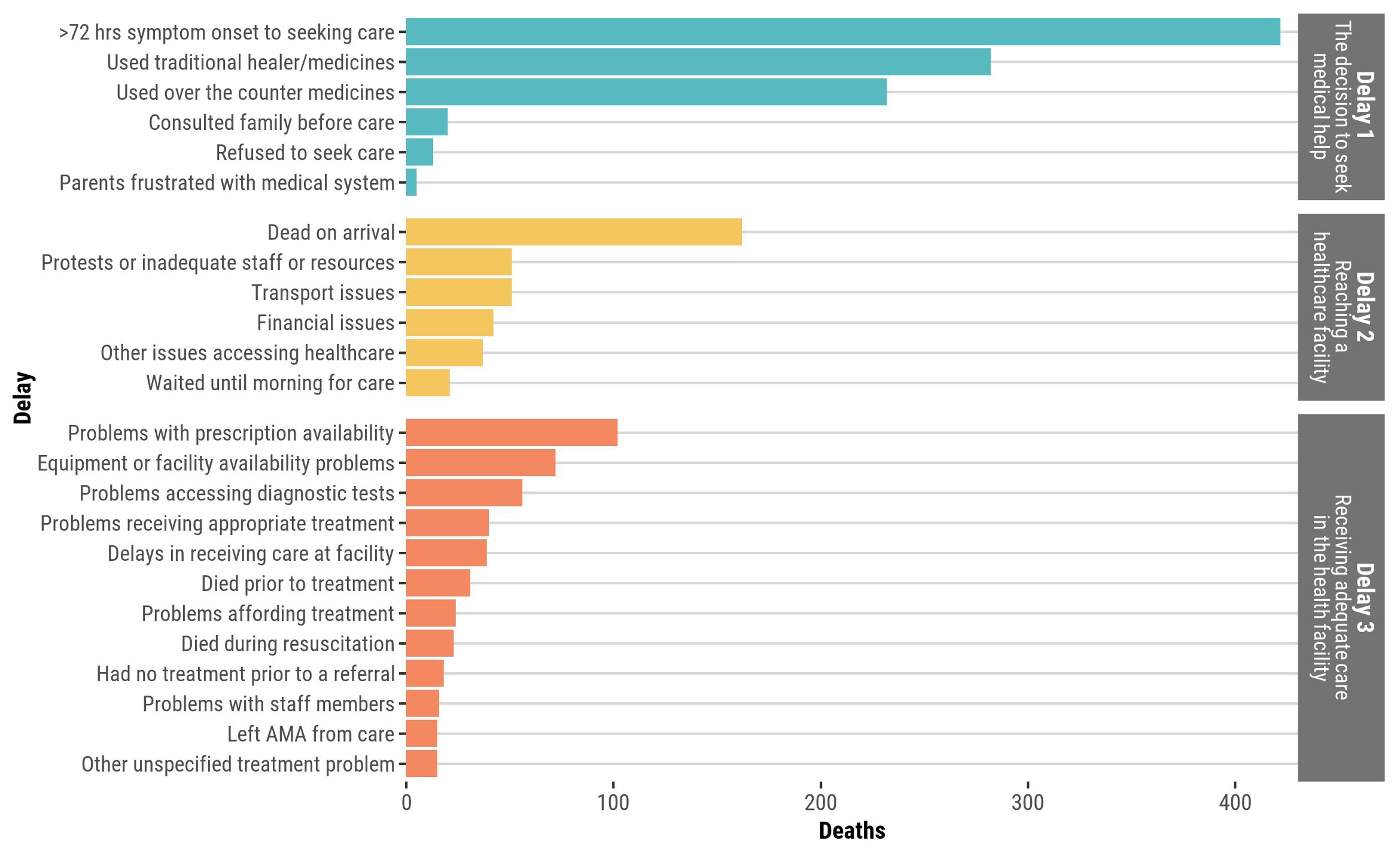
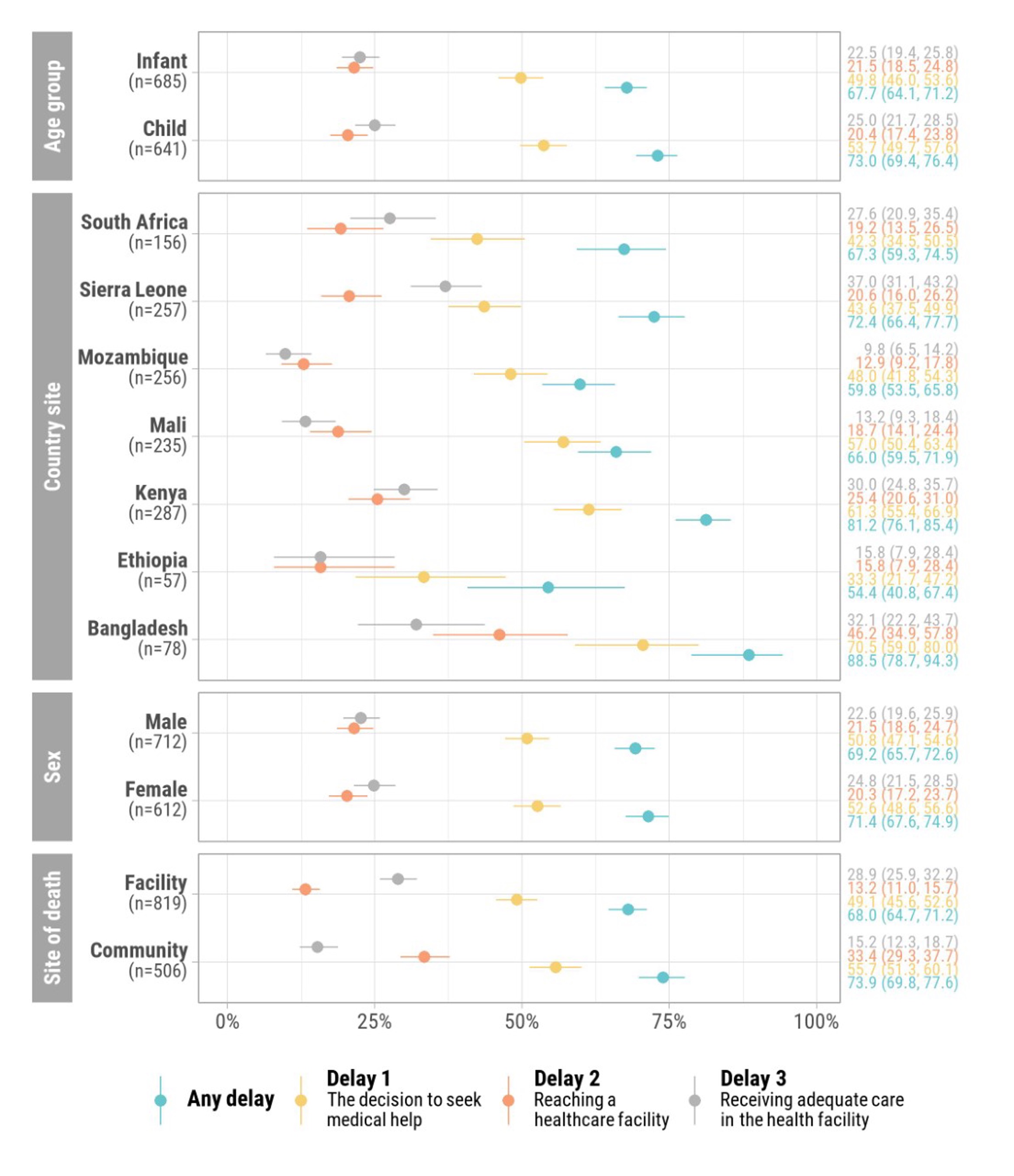
Results: We analyzed 1,326 deaths among infants and children. The majority had at least one identified delay (n=932, 70.3%) and over half (n=685, 51.7%) experienced delays in the home. Waiting >72 hours after illness recognition to seek any health care (n=422, 31.8%) was the most common delay followed by preferred initial use of traditional medicine (n=282, 21.3%) (Figure 1). Delays in transport were common: 192 (14.5%) infants and children presented to a healthcare facility dead on arrival. In healthcare facilities, indicated prescription medications were sometimes unavailable (n=104, 7.8%). Deceased children aged 12-59 months experienced more of any delay than infants aged 1-11 months (73.0% vs. 67.7%, P=0.041) (Figure 2). Waiting >72 hours after illness recognition to seek healthcare was more common among caregivers at sites in Bangladesh and Kenya than the other sites (Figure 3).
Conclusion(s): Community-based interventions that incorporate education on timely healthcare seeking after illness recognition have the potential to reduce mortality among infants and children. Health system strengthening is needed to provide timely transportation to healthcare facilities and appropriate medication availability in healthcare facilities.