Neonatal Neurology: Clinical Research
Neonatal Neurology 4: Clinical 4
95 - A fully automated bedside trend, Brain State of the Newborn (BSN), predicts the clinical outcome after perinatal asphyxia
Publication Number: 95.336
- SM
Saeed Montazeri Moghadam, MSc (he/him/his)
PhD student
University of Helsinki
Helsinki, Uusimaa, Finland 
Sampsa Vanhatalo, MD PhD (he/him/his)
Professor in Physiology
University of Helsinki
Helsinki, Uusimaa, Finland
Presenting Author(s)
First Author(s)
Background:
Long-term EEG monitoring is indicated by many guidelines, but it is hampered by the lack of resources for a continuous EEG review. We have recently developed a robust, deep learning -based algorithm (Brain State in the Newborn, BSN) that makes reliable interpretations and visualization of the EEG background activity [1]. The BSN is a continuous index that ranges from 0 (inactive) to 100 (fully continuous, age typical).
[1] Moghadam, S.M., et al., An automated bedside measure for monitoring neonatal cortical activity: a supervised deep learning-based electroencephalogram classifier with external cohort validation. Lancet Digit Health, 2022. 4(12): p. e884-e892.
Objective: We studied clinical utility of BSN in the fully automated interpretation of early EEG background after perinatal asphyxia. In particular, we examined the potential of BSN to predict clinical outcomes, such as death, infantile epilepsy, CP and a favorable outcome.
Design/Methods:
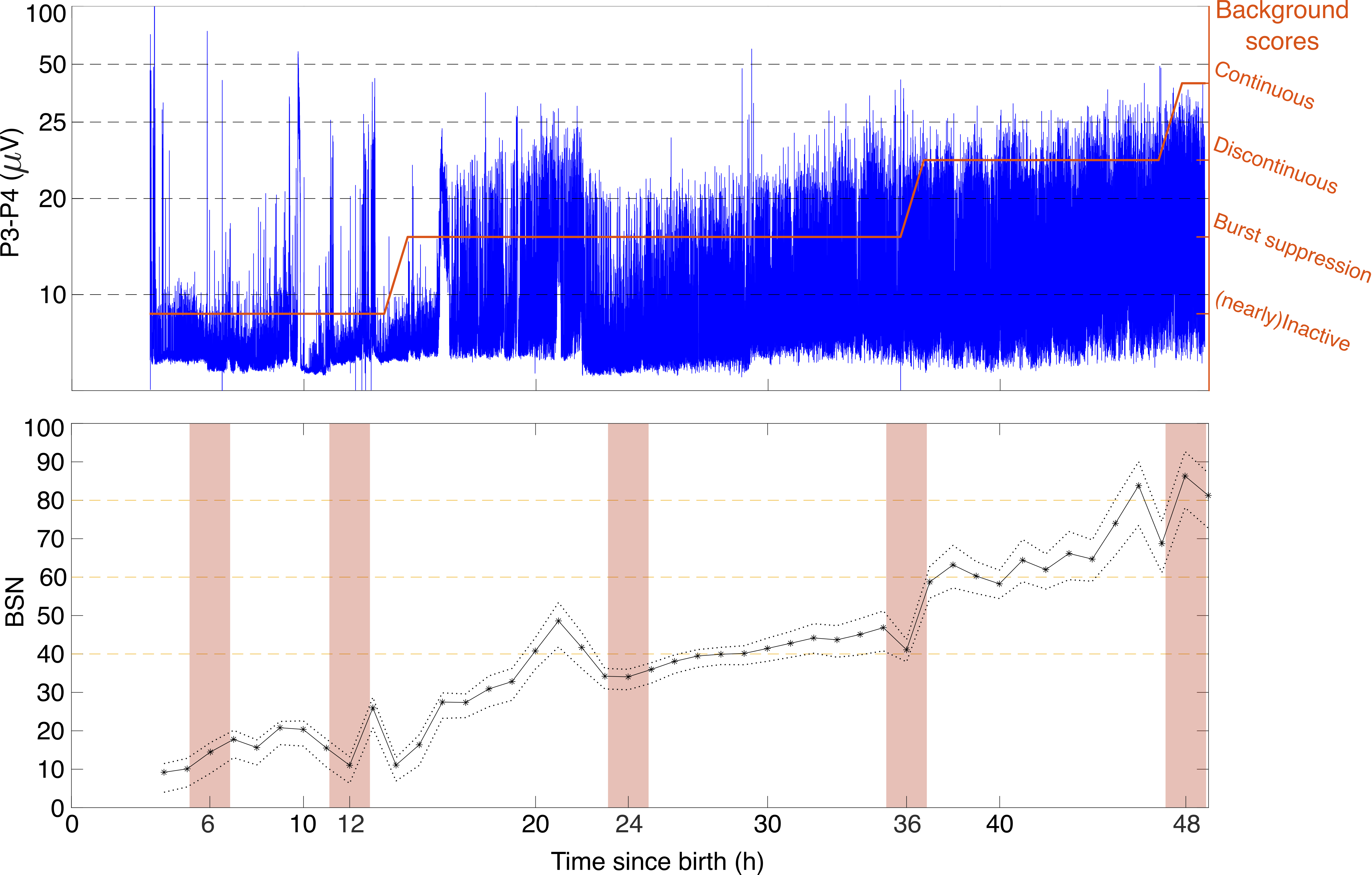
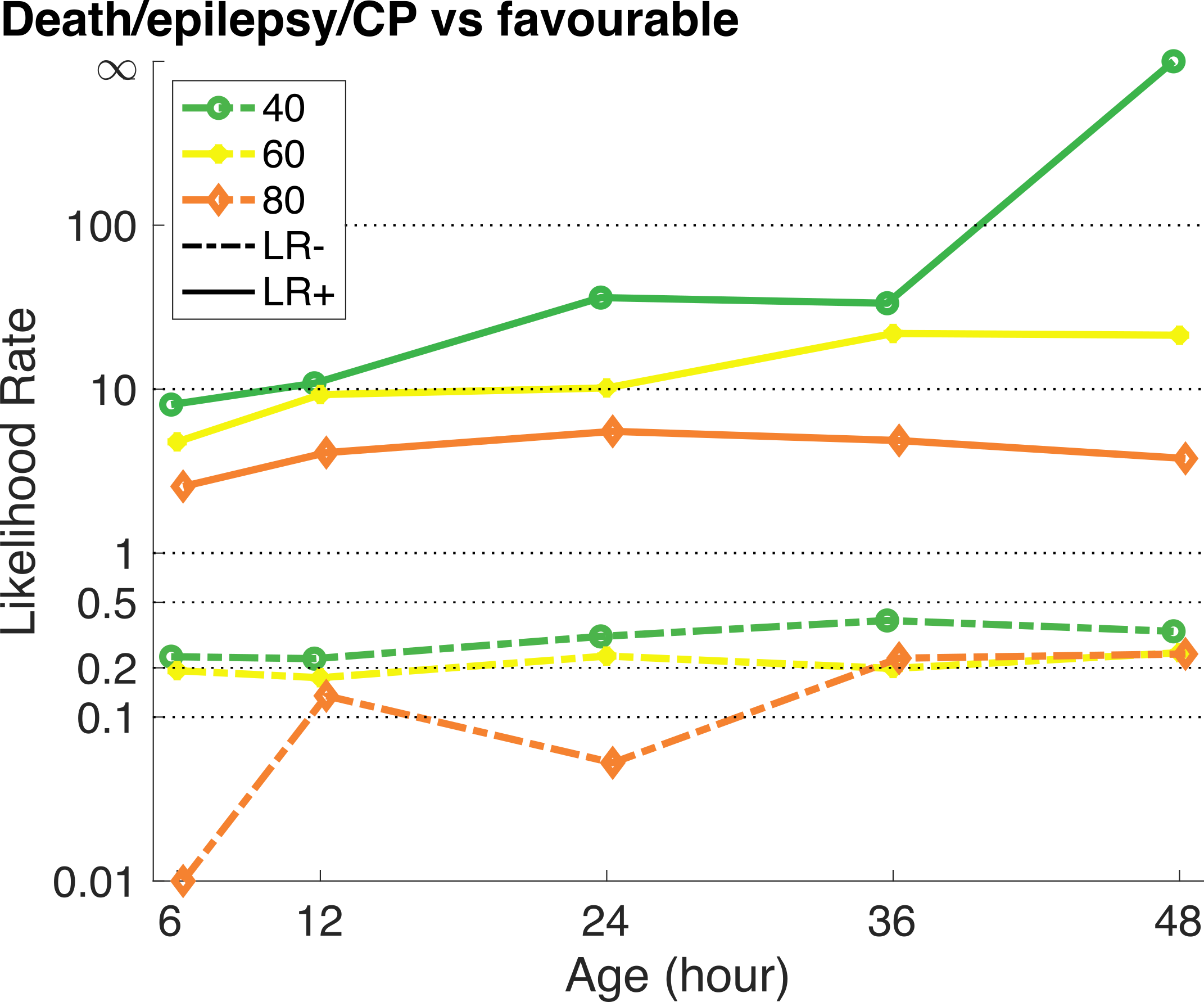
We re-analyzed a previously published cohort of N=80 full-term infants with moderate or severe HIE. The average BSN trends were computed from 4-channel (a)EEG recordings in 2-hour epochs between 6 and 48 hours of age (Fig 1). Clinical outcomes were: deceased (N=11), epilepsy (N=6), CP without epilepsy (N=7), and favorable (N=56). We then computed positive and negative likelihood ratios (LR+ and LR-, respectively) for the clinical outcomes and different BSN cut-off levels (40, 60, and 80). We defined LR+ for poor outcome (death, infantile epilepsy, and CP) when BSN value is lower than a threshold. The full BSN algorithm is available openly via cloud server (babacloud.fi).
Results:
BSN was successfully computed for the full EEG recordings (27-237 hours), providing an easy overview of background recovery (Fig 1). Comparison of the LR+ and LR- for different BSN thresholds showed a clear, expected trend over time. The lower BSN levels ( < 40) corresponded to a high LR+ for poor outcome, increasing markedly over time. The LR+ was clearly lower with higher BSN levels (Fig 2).
Conclusion(s):
The present findings show that BSN trend
-provides a convenient interpretation of the recovering cortical activity in HIE.
-allows an efficient clinical outcome prediction from early hours of life.
-overcomes many ambiguities related to the conventional, discrete EEG categories.
Future studies are needed to establish evidence-based, and context-sensitive limits for BSN to provide efficient clinical guidelines for using BSN in the clinical care.