Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 1
301 - Evaluating the Effect of Advanced Airway Type on Time to Effective Ventilation in a Neonatal Mock Code
Publication Number: 301.347

Shoshana Newman-Lindsay, MD MPH (she/her/hers)
Neonatal Perinatal Fellow
University of California Davis Health System (UC Davis) - Sacramento, CA
Sacramento, California, United States
Presenting Author(s)
Background:
Effective ventilation is crucial in neonatal resuscitation. Laryngeal Mask Airways (LMA's) can reduce the need for tracheal intubation (TI) and may improve time to effective ventilation. The use of LMA's has been shown to improve mortality in low resource countries. However, the current Neonatal Resuscitation Program (NRP) recommends use of a LMA only if facemask ventilation is unsuccessful and TI is not feasible or unsuccessful.
Resident physicians are trained in neonatal resuscitation, though most go onto careers in which resuscitating a newborn is a low-frequency event. TI is a technically challenging skill with few opportunities to practice.
Objective: To determine if resident physicians will be able to provide more timely invasive positive pressure ventilation in a simulated resuscitation when placing a LMA or performing TI.
Design/Methods:
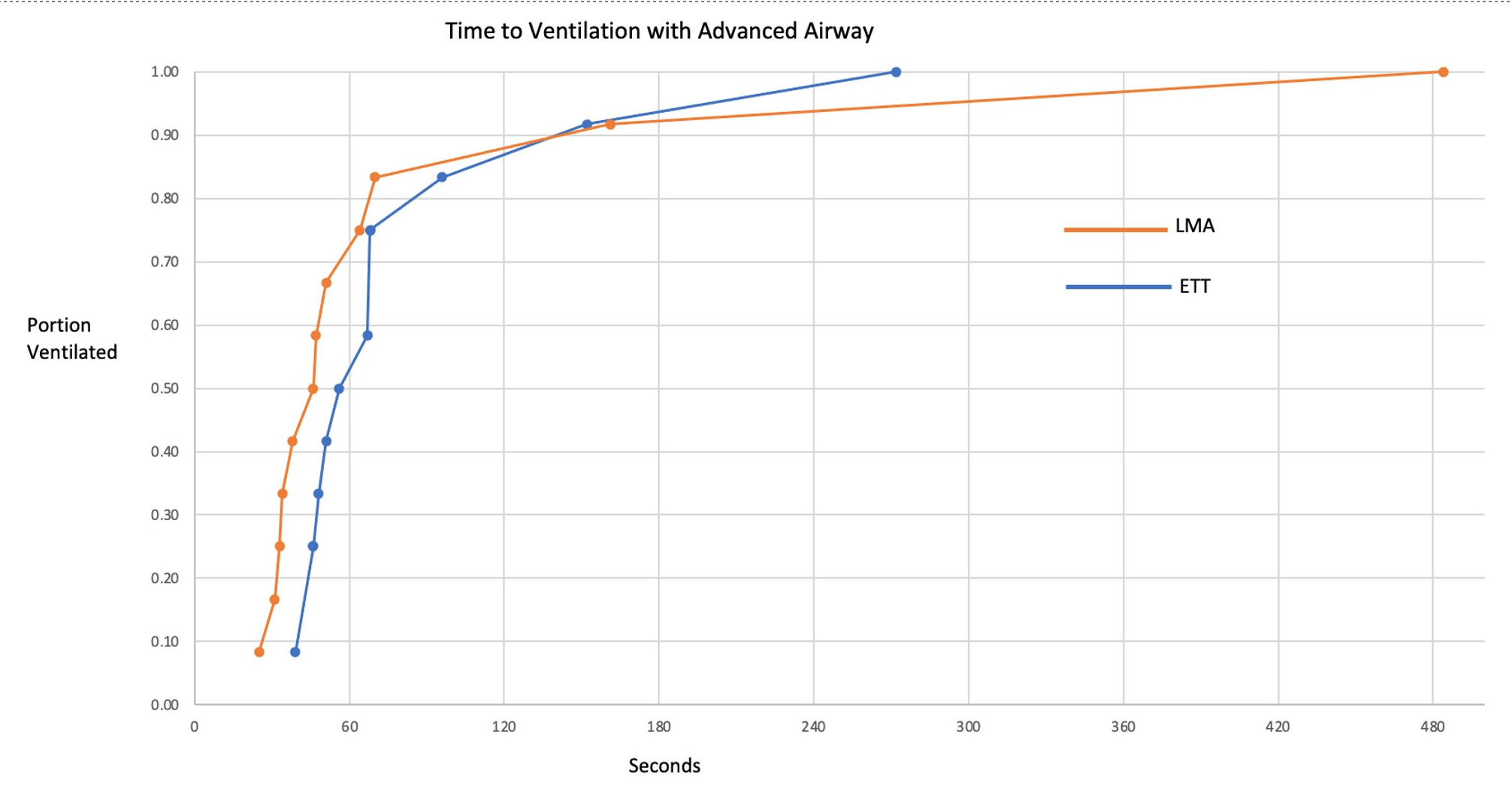
We recruited NRP-trained resident physicians, targeting a sample size of 24 based on average time to TI of 56 seconds and LMA placement of 36 seconds. After orientation to the Gaumard Code Blue III Neonatal manikin and practice with both airways as desired, participants were randomized to TI or LMA placement and participated in a mock code in which the neonate remained apneic with a heart rate of 60-80 until advanced airway was successfully placed. Time to effective ventilation was determined by the time interval from when the airway provider announced intent to place the advanced airway until delivery of ten breaths at targeted tidal volume, as measured by the manikin’s software (fig 1). Participants were surveyed on their confidence and ease with the airway. UC Davis IRB found study exempt.
Results:
Twenty-four residents participated, twelve in each group(Table 1). The mean time to effective ventilation was 90.3 (SD 123) seconds for the LMA group and 84.1 (SD 63) seconds for the TI group. First attempt success rates were the same at 10/12 (83%).However all of those unsuccessful on first attempt at TI succeeded on second attempt, while the two participants that were initially unsuccessful in their LMA placement required three and four attempts. All participants agreed or strongly agreed that their airway type was easy to insert, and all reported improved confidence with neonatal resuscitation after participation.
Conclusion(s):
Robust evidence supports use of LMA’s in low resource settings, however these benefits have not been translated in this or other manikin studies in the United States. The difficulty in accurately mimicking the dynamic airway of a distressed neonate with a manikin may explain part of this gap and warrants further exploration.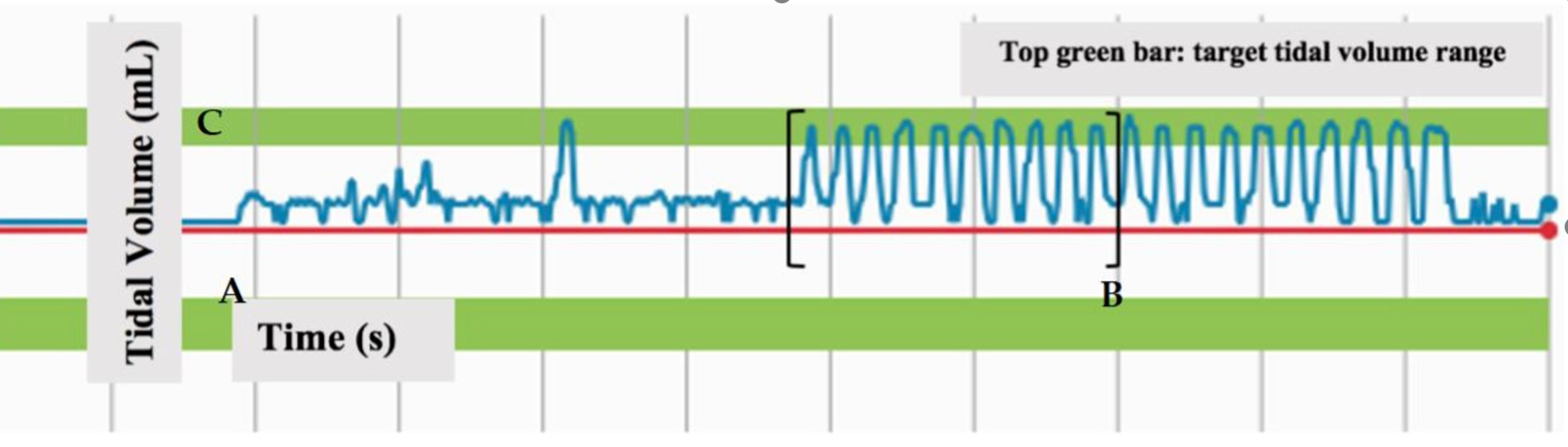
.png)