Neonatal Pulmonology
Neonatal Pulmonology 2: BPD Clinical
257 - Post-Discharge Exposure to Diuretics, Inhaled Steroids, Inhaled Bronchodilators, and Anti-Reflux Medications: A Secondary Analysis of the PENUT Trial Cohort
Publication Number: 257.34

Kaashif A. Ahmad, MD (he/him/his)
Research Director of Neonatal Clinical Trials
Pediatrix Medical Group
San Antonio, Texas, United States
Presenting Author(s)
Background:
Bronchopulmonary dysplasia (BPD) remains the most frequent complication of extreme prematurity. Though infants with BPD have substantial medication exposure during their hospital course, little is known about medication exposures after discharge.
Objective:
To describe medication exposure among premature infants with and without BPD after NICU discharge through 2 years of age.
Design/Methods:
A secondary analysis of the Preterm Epo Neuroprotection Trial (PENUT), a randomized controlled trial of erythropoietin for neuroprotection in infants 24-27 weeks’ gestation. Infants surviving through discharge had survey data collected at 4-, 8-, 12-, 18-, and 24-months corrected age (CA) regarding active medication utilization. We used descriptive statistics and graphic illustrations to describe baseline maternal and infant characteristics.
Results:
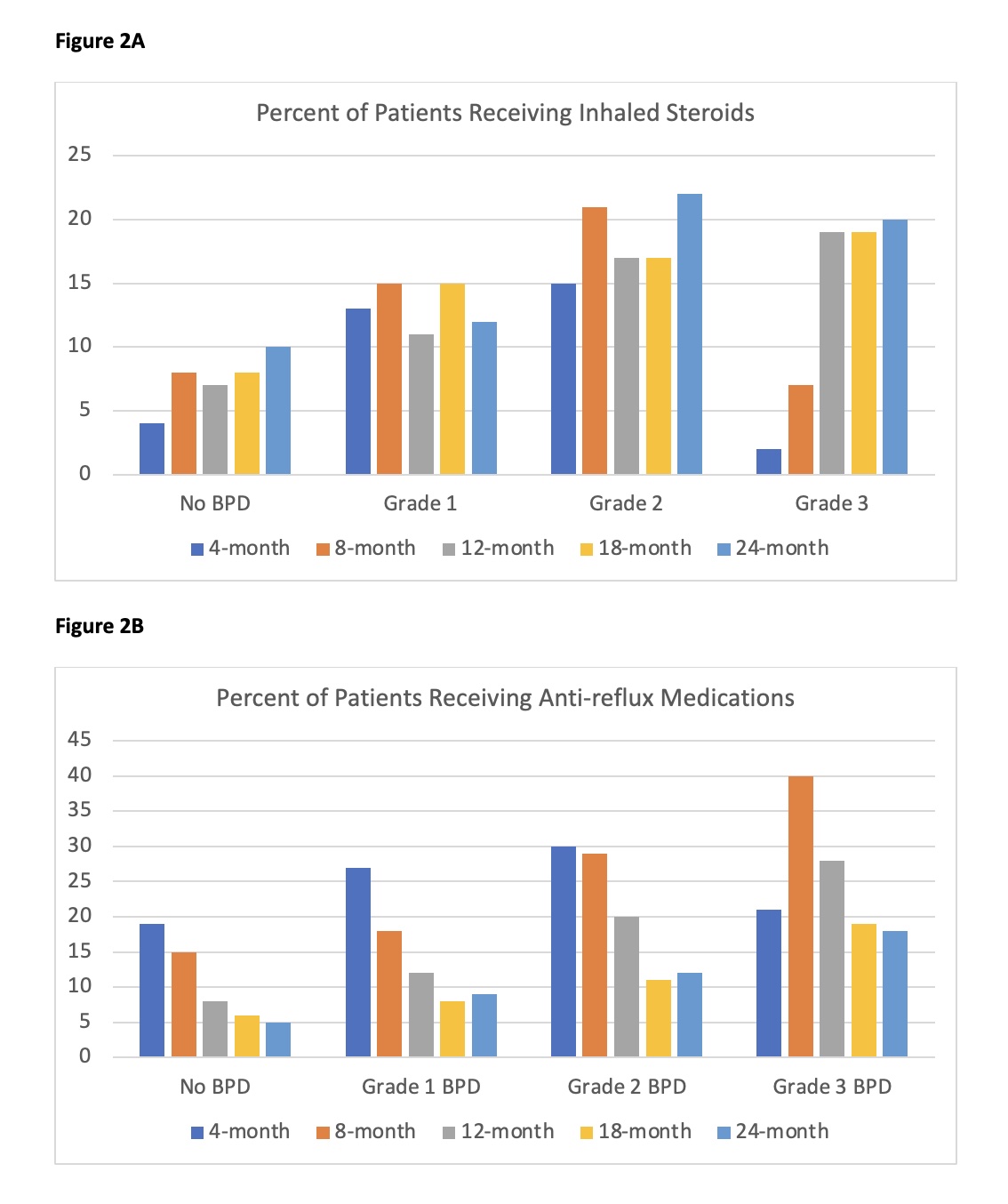
Of 941 randomized patients, 874 received an assessment at 36-weeks for BPD. Of these, 320 (37%) had no BPD, 286 (33%) had Jensen Grade 1 BPD, 212 (24%) Grade 2, and 56 (6%) Grade 3. Medication exposure data was successfully obtained for 811 patients (93%) at 4-months CA, 802 (92%) at 8-months CA, 796 (91%) at 12-months CA, 781 (89%) at 18-months CA, and 761 (87%) at 24-months CA.
Compared to those without BPD, infants with Grade 3 BPD more frequently experienced severe necrotizing enterocolitis, intraventricular hemorrhage, retinopathy of prematurity, and periventricular leukomalacia. These infants also more frequently received diagnoses of cerebral palsy or severe neurodevelopmental impairment at 2-years of age (Table 1).
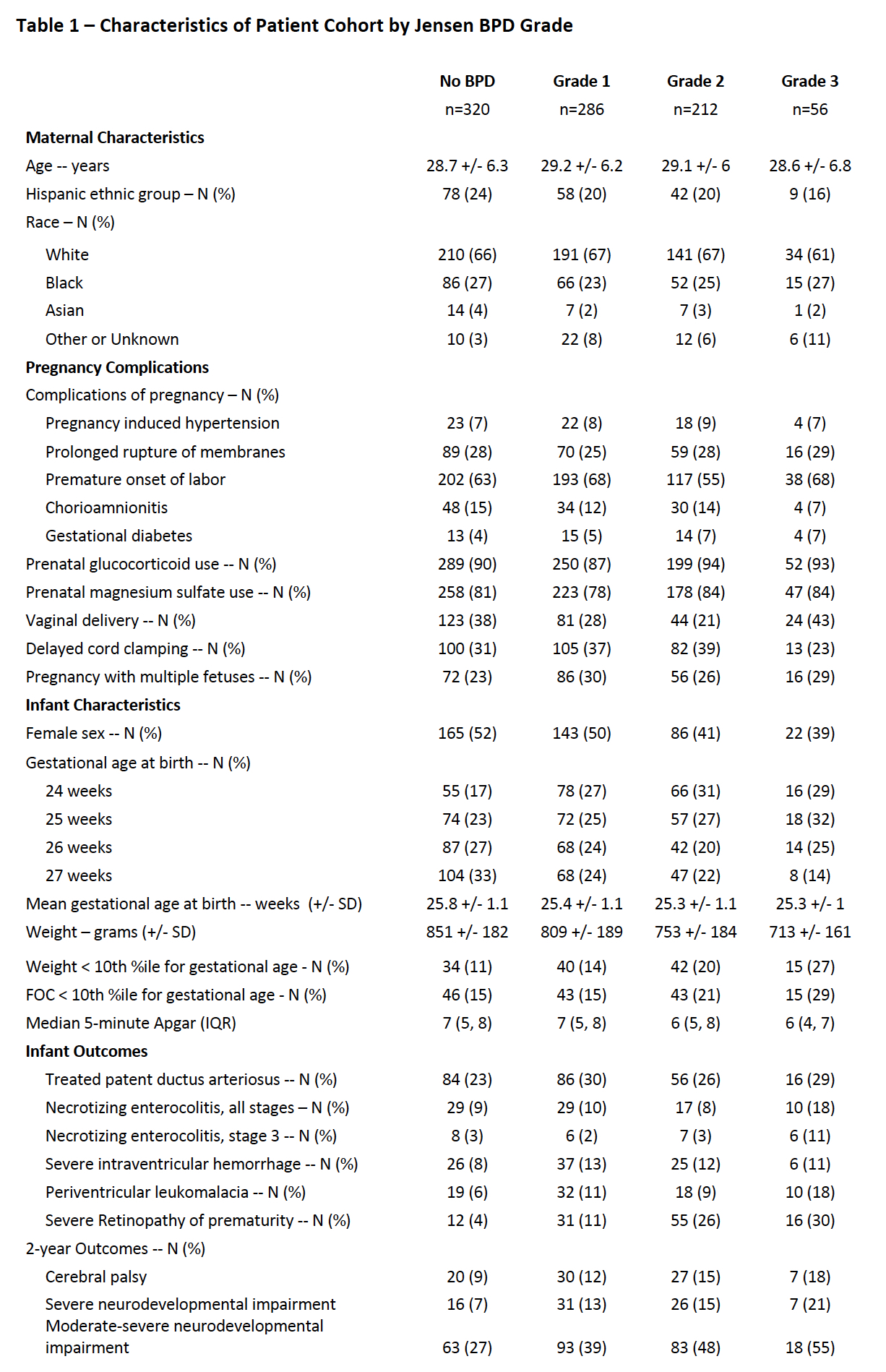
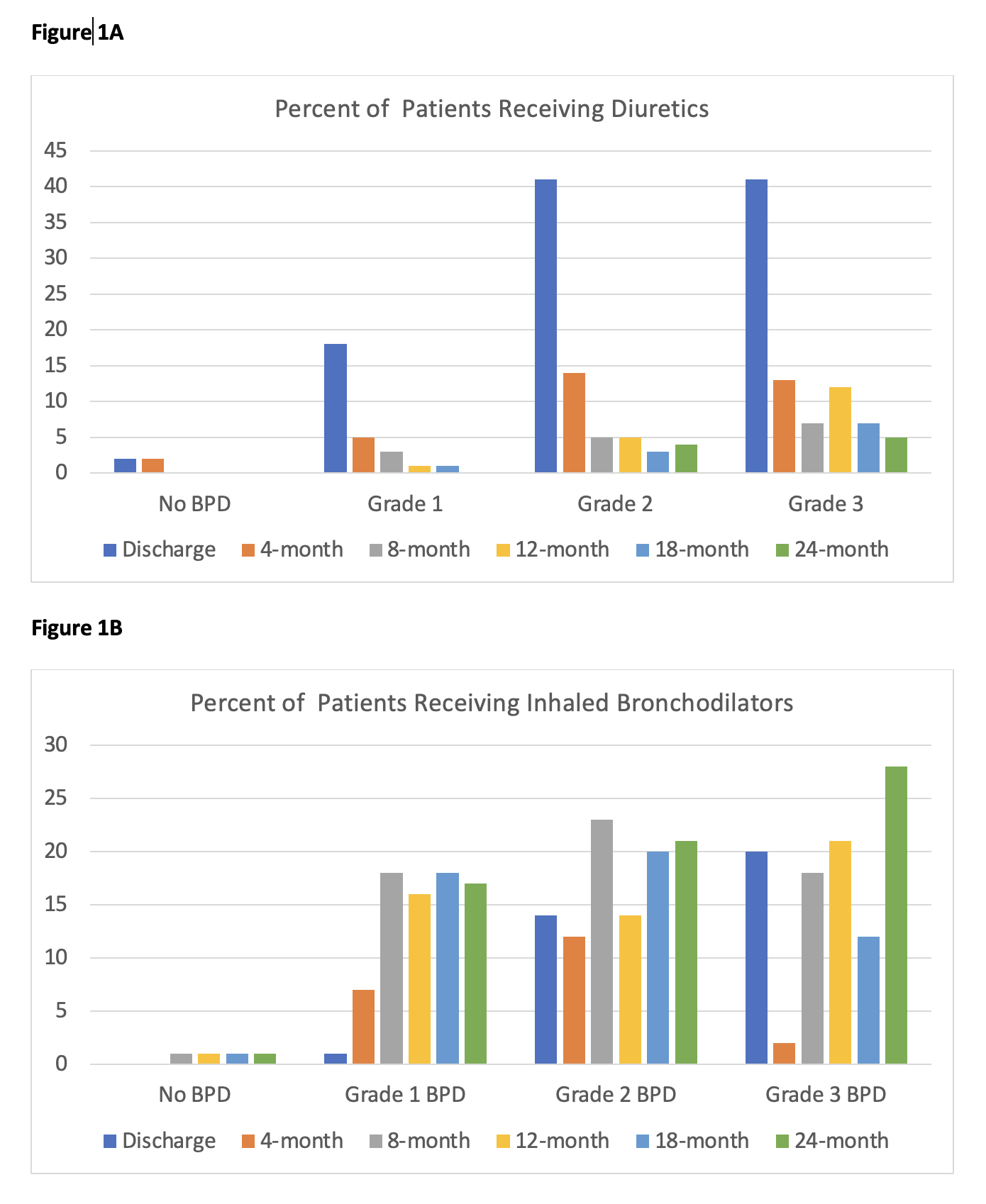
Infants with BPD commonly received oral diuretics at discharge with a significant decrease in utilization by 4-months CA (Fig 1A). Conversely, while inhaled bronchodilators were less commonly utilized at discharge, use among some infants with BPD persisted through 2-years CA (Fig 1B). We found that use of inhaled steroids gradually increased through the first 2-years (Fig 2A) whereas anti-reflux medication use peaked at 4-months CA for infants with < Grade 3 BPD and then gradually decreased (Fig 2B).
Conclusion(s):
Infants diagnosed with BPD are frequently exposed to classes of medications in early childhood with little proven long-term efficacy. Further investigation is needed into factors influencing outpatient prescribing practices and the long-term impact of exposure to these medications.