Nephrology: Transplant
Nephrology 4: Transplant
33 - Dyslipidemia in Pediatric Kidney Transplant Recipients on Steroid-Avoidance Maintenance Immunosuppression
Publication Number: 33.349
.jpg)
Emily E. Zangla, DO (she/her/hers)
Pediatric Nephrology Fellow, PGY-5
University of Minnesota Medical School
Minneapolis, Minnesota, United States
Presenting Author(s)
Background:
Dyslipidemia is a known, modifiable risk factor for cardiovascular disease in adults with a kidney transplant. However, the prevalence of dyslipidemia in pediatric kidney transplant recipients under modern immunosuppression remains unknown.
Objective:
We aimed to determine the prevalence, severity, and risk factors for dyslipidemia in pediatric kidney transplant recipients on steroid-avoidance maintenance immunosuppression.
Design/Methods:
One hundred and thirteen pediatric kidney transplant recipients (≤21 years) on steroid-avoidance maintenance immunosuppression underwent dyslipidemia screening per the institutional protocol between 1/1/2020 and 9/30/2022. Dyslipidemia was defined according to the criteria in Table 1. Patients with abnormal lipid profiles but unknown fasting status were excluded (n=17). We compared continuous and categorical variables using the Wilcoxon-rank sum and Fisher’s exact tests, respectively. Risk factors for dyslipidemia were evaluated using multivariable logistic regression.
Results:
Our final analysis cohort included 96 patients with a median posttransplant time of 2.5 years (IQR: 1.3 to 5.4 years). Fifty-two (54.2%) patients had dyslipidemia, and thirty-one of them (59.6%) had more than one lipid abnormality. The baseline characteristics were similar between patients with and without dyslipidemia (Table 2). Of the patients with dyslipidemia, 26.9% had hypercholesterolemia (median: 218.5mg/dL), 88.5% had hypertriglyceridemia (median: 188.5mg/dL), 59.6% had low HDL (median: 30mg/dL), 15.4% had elevated LDL (median: 155.5mg/dL), and 17.3% had elevated non-HDL cholesterol (median: 182mg/dL). We found a significant correlation between total cholesterol and BMI (r = 0.34, p = 0.014). After multivariable adjustment, BMI percentile (p=0.07), Native American race (p=0.08), and donor type (p=0.07) approached statistical significance as independent risk factors for dyslipidemia (Table 3). Among patients with dyslipidemia, 65.4% had hypertension, 47.2% had left ventricular hypertrophy, and 13.7% had insulin-treated post-transplant diabetes. Only 36.5% (n=19) received an intervention for dyslipidemia; 12 were referred for dietary modifications, 6 were referred to a lipid specialist, and one received statin therapy.
Conclusion(s):
Dyslipidemia is highly prevalent among pediatric kidney transplant recipients on steroid-avoidance maintenance immunosuppression. Only one-third of patients received an intervention for dyslipidemia. Larger studies are needed to determine the risk factors and long-term outcomes of dyslipidemia in pediatric transplant recipients.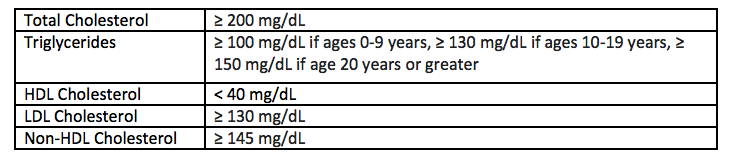
.png)
.png)
