Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 1
300 - Neonatal Resuscitation Program (NRP) Guidelines and Timing of Actual Resuscitation Events at a Level III NICU: Understanding Deviations
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 300
Publication Number: 300.347
Publication Number: 300.347
Praveen kumar Boddu, Children's Hospital of Michigan, Livonia, MI, United States; Monika Bajaj, Children's Hospital of Michigan, Detroit, MI, United States; Pradeep kumar Velumula, Mercy One Waterloo Medical Center, Waterloo, IA, United States; Girija Natarajan, Children's Hospital of Michigan, Detroit, MI, United States; Sanket Jani, Children's Hospital of Michigan, Detroit, MI, United States; Jorge Lua, Children's Hospital of Michigan, Troy, MI, United States; Nithi Fernandes, Children's Hospital of Michigan, Detroit, MI, United States; Sanjay Chawla, Children's Hospital of Michigan, TROY, MI, United States
Praveen kumar Boddu, MBBS, MD (he/him/his)
Neonatal-Perinatal Medicine Fellow
Children's Hospital of Michigan
Livonia, Michigan, United States
Presenting Author(s)
Background: There are limited data regarding the actual timing of key resuscitation events in the delivery room (DR) based on the NRP algorithm
Objective:
- To describe the timing of key resuscitation events in the NRP guidelines for neonates receiving resuscitation in the DR.
- To assess whether the presence of a neonatal resuscitation team prior to birth was associated with an improved timing of key resuscitation events.
- To assess factors associated with a significant delay in the timing of key resuscitation events in DR.
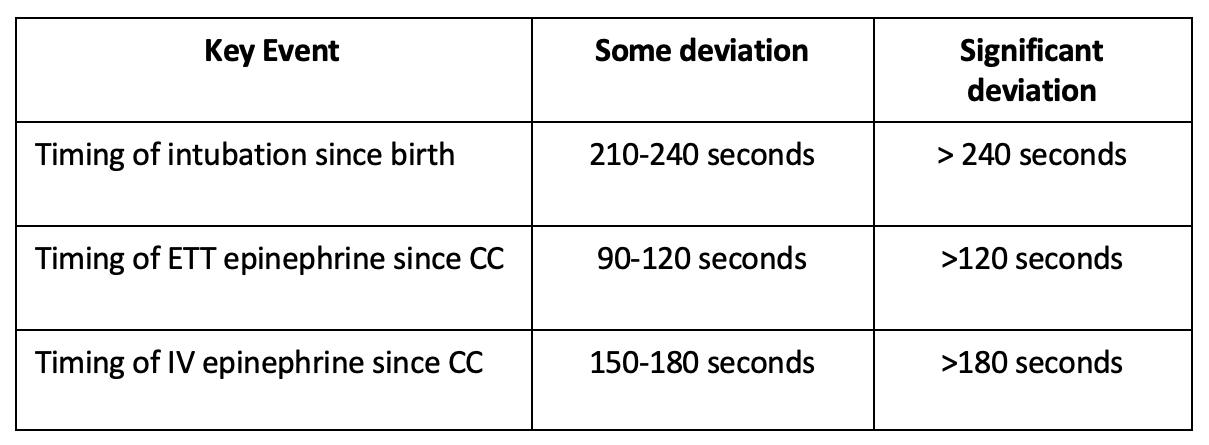
Design/Methods: A retrospective chart review included neonates born between January 2015 and May 2022 who received chest compressions (CC) in the DR. The key resuscitation events were assigned into 3 categories based on timing, 1) No deviation, 2) Some deviation and 3) Significant deviation (Table 1). The primary outcome was significant deviation in any of the key events. The key resuscitation events studied were a) time to secure an alternate airway, b) time of endotracheal (ET) epinephrine (EPI) c) timing of intravenous (IV) EPI. Frequency of significant deviation was compared for deliveries with and without the presence of neonatal team prior to delivery. All high risk deliveries are attended by a fellow, residents, respiratory therapist, nurse and attending neonatologist
Results: A total of 51 neonates met the inclusion criteria; the mean (SD) gestational age was 30.2 ±6.6 weeks. The neonatal team was present prior to delivery in 38 (74.5%); From the time of birth, PPV was initiated at 57.4 ± 24.8 seconds, an alternate airway was secured at 4.2 ± 5.9 minutes (Median 2.5 IQR=1-5) and CC were started at 5.4 ± 5.2 minutes (median 4 IQR=2-7). The mean time from initiation of resuscitation to placement of an umbilical venous catheter (UVC) was 16 ± 8.6 minutes (Median 14 IQR=9-20). From the time of initiation of CC, ET EPI was administered at 4 ± 3 minutes (median 2.5 IQR= 2-5) and IV EPI was administered at a mean time of 10.9 ± 5.2 minutes (median 10; IQR= 7-16). An alternate airway was secured before the initiation of CC in 69.2% of deliveries when neonatal team was present prior to delivery as compared to 23.7% when not present (p= 0.003). The primary outcome (significant deviation in any of the key events) occurred in 84.8%.
Conclusion(s): The adherence to NRP specified guidelines for timely initiation of key resuscitation events may be difficult to achieve in the DR. The occurrence of significant delays in many key resuscitation events from a large level III NICU with multiple providers attending deliveries provides data on the practical limitations on the adherence to NRP guidelines.
.jpg)
.jpg)
