Neonatal Quality Improvement
Neonatal Quality Improvement 3
725 - Optimizing the Time to Antibiotic Administration in Late Onset Neonatal Sepsis
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 725
Publication Number: 725.342
Publication Number: 725.342
Alexandria D. Cremeans, Wake Forest Baptist Health - Brenner Children's Hospital, Winston-Salem, NC, United States; Cherrie Welch, Wake Forest Baptist Health - Brenner Children's Hospital, Winston Salem, NC, United States; Linda B.. Esposito, Wake Forest Baptist Health - Brenner Children's Hospital, Winston-Salem, NC, United States; Tonya Oliver, Atrium Health Wake Forest Baptist, Pfafftown, NC, United States; Courtney J. Perry, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, winston-salem, NC, United States
Alexandria D. Cremeans, MD (she/her/hers)
Fellow
Wake Forest Baptist Health - Brenner Children's Hospital
Winston-Salem, North Carolina, United States
Presenting Author(s)
Background: Neonatal sepsis is associated with a higher risk of mortality, increased length of hospitalization, and neurologic impairment. Delayed time to antibiotic administration is an independent risk factor for sepsis associated mortality. The accepted standard is administration of antibiotics within one hour of intent. The choice of empiric antibiotics must be tailored to bacteria common in the setting. The implementation of a standardized “Code Sepsis” process will reduce the time of antibiotic administration and will improve appropriate empiric antibiotic selection.
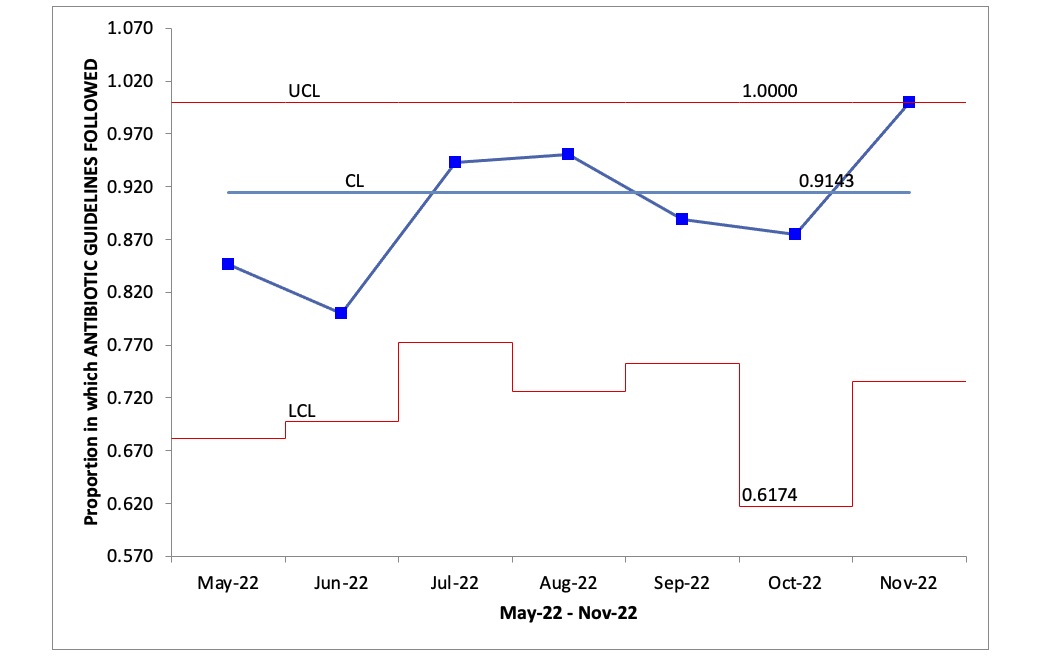
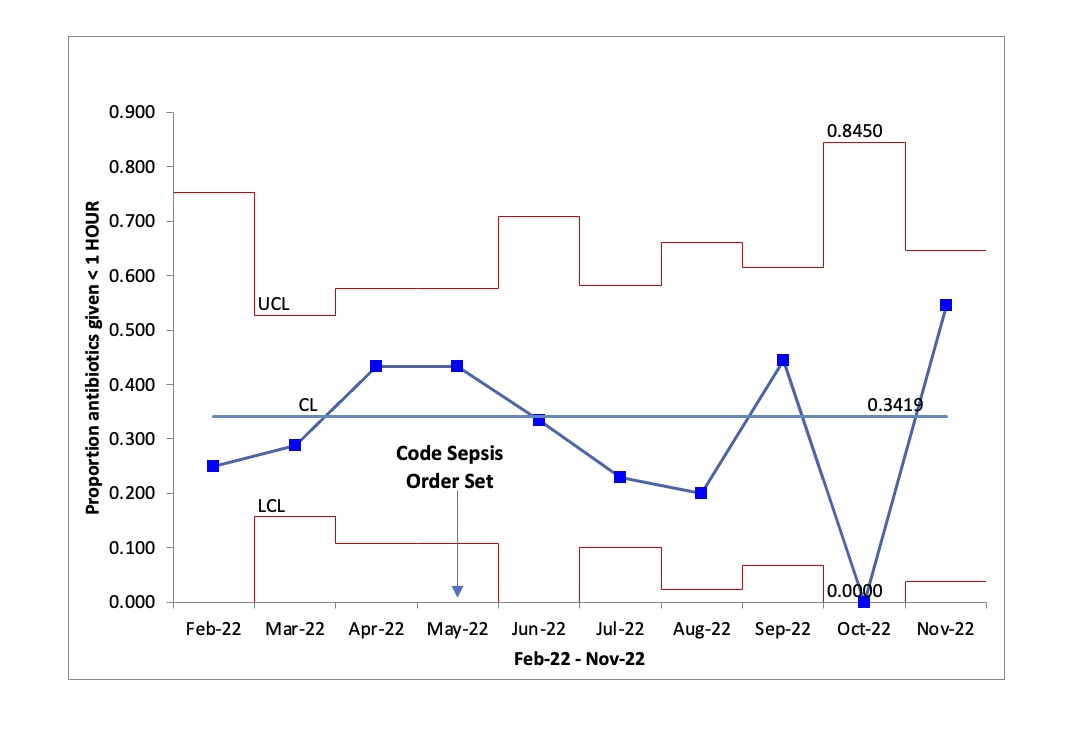
Objective: The primary aim of this initiative is to increase the percentage of infants who receive antibiotics within one hour of intent from a baseline of 33% to > 80%. The secondary aim is to achieve compliance with our “Code Sepsis Antibiotic Selection Guidelines” in > 80% of cases. Both aims are to be achieved within 12 months of the start of the initiative.
Design/Methods: A multidisciplinary team utilized the “Model for Improvement” to develop, test and implement processes to facilitate appropriate empiric antibiotic selection and to reduce time of antibiotic administration. We implemented a “Code Sepsis” order set in which all antibiotics are ordered “STAT” and that includes a decision aid for appropriate selection of empiric antibiotics. Additional methods have included education sessions for team members, reminder signage, performance feedback and incentives. Outcome measures include compliance with antibiotic selection guidelines and duration of time from antibiotic order to administration. Our primary p</span>rocess measure is compliance with using the “Code Sepsis” order set. The balance measure is the inability to obtain a blood culture prior to antibiotic administration. Infants who are administered antibiotics for early onset sepsis or for primarily surgical concerns are excluded from the analyses.
Results: On average 27 sepsis evaluations occur per month in our unit. We are currently in the seventh month of this initiative. So far, there has not been a significant difference in the percentage of infants receiving antibiotics within one hour. However, compliance using the “Code Sepsis” order set and selection of the recommended antibiotics has been 62% and 91%, respectively since implementation.
Conclusion(s): The use of our “Code Sepsis” order set has resulted in reduced variability and improved appropriate antibiotic selection. Further efforts are underway to determine and remove remaining barriers to administering antibiotics within one hour of intent.