Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 1
299 - Characteristics of Nonvigorous Newborns Born Through Meconium-Stained Amniotic Fluid
Publication Number: 299.347
.jpg)
Yumna Furqan, B.S
Medical Student
Texas A&M Health Science Center College of Medicine
Dallas, Texas, United States
Presenting Author(s)
Background:
Meconium-stained amniotic fluid (MSAF), found in 8 to 10% of all deliveries, is a common perinatal concern. Approximately 10% of the infants born through MSAF are reported to be nonvigorous if presented with depressed breathing and decreased tone immediately after birth. Neonatal Resuscitation Program discouraged routine endotracheal suctioning for these infants since the publication of 7th edition. However, the perinatal factors affecting the nonvigorous status of the newborn and the characteristics after birth remain ill-defined in the new era of no routine endotracheal suctioning for meconium.
Objective:
The purpose of this study was to define the perinatal factors affecting the nonvigorous status and the characteristics immediately after birth of the newborns born through MSAF.
Design/Methods:
This multi-center retrospective cohort study conducted through chart reviews included infants ≥ 35 weeks' gestation born through MSAF between the time period of January 1, 2017 and December 31, 2019. The infants who were nonvigorous immediately after birth were compared to those who were vigorous.
Results:
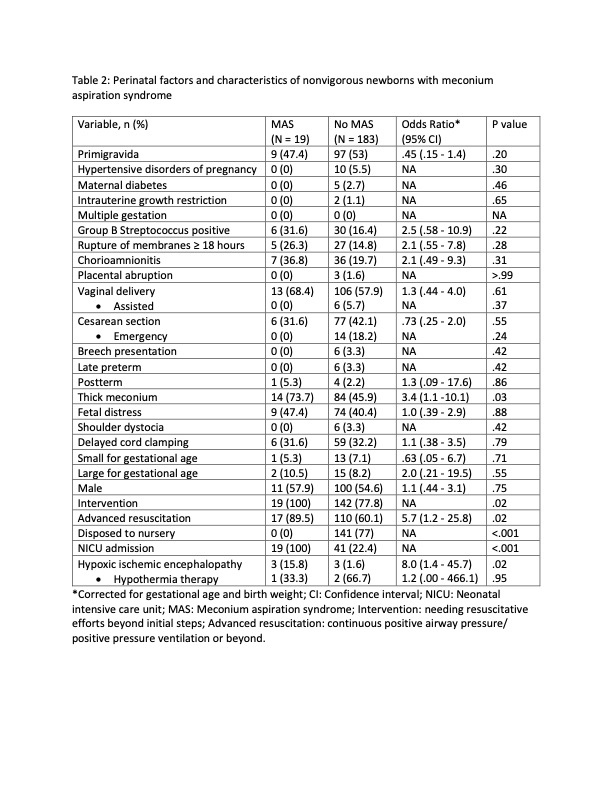
During the three-year study period, out of 18,449 infants born ≥ 35 weeks' gestation, 2213 (12%) were meconium-stained and eligible. Out of those, 202 (9%) were nonvigorous at birth. Logistic regression after correcting for gestational age and birth weight revealed the following perinatal factors significantly influenced the nonvigorous status of the newborn: rupture of membranes ≥ 18 hours, chorioamnionitis, placental abruption, assisted vaginal delivery, emergency cesarean section, thick meconium, fetal distress and shoulder dystocia. Significantly higher proportion of nonvigorous infants received intervention (needing resuscitative efforts beyond initial steps) or advanced resuscitation (continuous positive airway pressure/ positive pressure ventilation or beyond) in the delivery room. The incidence of neonatal intensive care unit admission, meconium aspiration syndrome (MAS) and hypoxic ischemic encephalopathy (HIE) were significantly higher in the nonvigorous group compared to vigorous group. (Table 1). On secondary analysis, the perinatal factor significantly affecting the diagnosis of MAS in nonvigorous infants was thick meconium. (Table 2)
Conclusion(s):
Compared to infants born vigorous, nonvigorous meconium-stained infants were at higher risk for the development of MAS and HIE. The information on the perinatal factors influencing the nonvigorous status and MAS may help guide the management of these infants..jpg)