Nephrology: Clinical
Nephrology 5: CKD/ Diversity and Equity in Kidney Health
47 - Assessment of the Spectrum of Kidney Injury During Therapy for Pediatric Acute Leukemia
Publication Number: 47.35
Wendy C. Hsiao, MD (she/her/hers)
Pediatric Nephrology Fellow
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States- YL
Yimei Li, PhD
Perelman School of Medicine at the University of Pennsylvania
Philadelphia, Pennsylvania, United States - KG
Kelly D. Getz, PhD, MPH (she/her/hers)
University of Pennsylvania
Philadelphia, Pennsylvania, United States - LC
Lusha Cao, PhD, MS (she/her/hers)
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States - MS
Michael Scheurer, PhD, MPH (he/him/his)
Baylor College of Medicine
Houston, Texas, United States - EK
Edward M. Krause, M.S. Health Informatics (he/him/his)
Children's Hospital of Philadephia
Philadelphia, Pennsylvania, United States - RA
Richard Aplenc, MD PhD
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States - MD
Michelle Denburg, MD, MSCE
Associate Professor of Pediatrics and Epidemiology
Childrens Hospital of Philadelphia, Perelman School of Medicine at the University of Pennsylvania
Philadelphia, Pennsylvania, United States - TM
Tamara P. Miller, MD, MSCE
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
First Author(s)
Co-Author(s)
Background: Children with acute lymphoblastic and myeloid leukemia (ALL, AML) are at increased risk of acute kidney injury (AKI) and acute kidney disease (AKD), which may lead to chronic kidney disease (CKD). The chemotherapy course-specific prevalence of AKI is unknown in this population. Differences in ascertainment using Kidney Disease Improving Global Outcomes (KDIGO) or Common Terminology Criteria for Adverse Events (CTCAE) definitions may lead to challenges in investigating kidney injury.
Objective:
To describe the course-specific and overall prevalence of AKI, AKD without AKI, and CKD in children with ALL and AML using KDIGO and CTCAE definitions.
Design/Methods: Retrospective study of electronic health record data from patients treated for ALL or AML (2010-2018) at Children’s Hospital of Philadelphia, Children’s Healthcare of Atlanta, and Texas Children’s Hospital. Infant ALL, Down Syndrome AML, and incomplete courses were excluded. Patients were followed from time of study site entry including diagnosis through chemotherapy completion and were censored at end of therapy, death, relapse, conditioning for stem cell transplant, or leaving a study site. AKI was reported according to: 1) KDIGO, 2) KDIGO plus absolute serum creatinine value >0.5 mg/dL (AKI+0.5) to account for low baseline creatinine, and 3) CTCAE version 5 definitions. KDIGO AKD prevalence without AKI+0.5 was determined. CKD prevalence was defined as estimated glomerular filtration rate < 90 mL/min/1.73m2 for >90 days or by CTCAE criteria.
Results: 1216 ALL patients and 203 AML patients were included. During therapy, 84%, 47%, and 25% of ALL patients met criteria for AKI at least once using KDIGO AKI, KDIGO AKI+0.5, and CTCAE criteria, respectively (Table 1). Induction and interim maintenance had the highest prevalence of AKI among the ALL courses. AKD without AKI+0.5 occurred in 14% and CKD occurred in 2% (n=18) of ALL patients overall. In AML, 74%, 44%, and 32% met criteria for AKI using KDIGO AKI, KDIGO AKI+0.5, and CTCAE criteria, respectively (Table 2). Induction I had the highest prevalence of AKI. AKD without AKI+0.5 occurred in 20% and CKD occurred in 2% (n=4) overall. All CKD was CTCAE Grade 1/Stage 2 CKD.
Conclusion(s): The prevalence of AKI and AKD without AKI during therapy was substantial. Prevalence estimates of AKI varied widely based on which criteria were used, with CTCAE being the most conservative. KDIGO criteria may overestimate AKI in this population, perhaps due to low baseline creatinine values in a predominantly young population. More investigation is needed on how to optimally determine kidney injury in this population.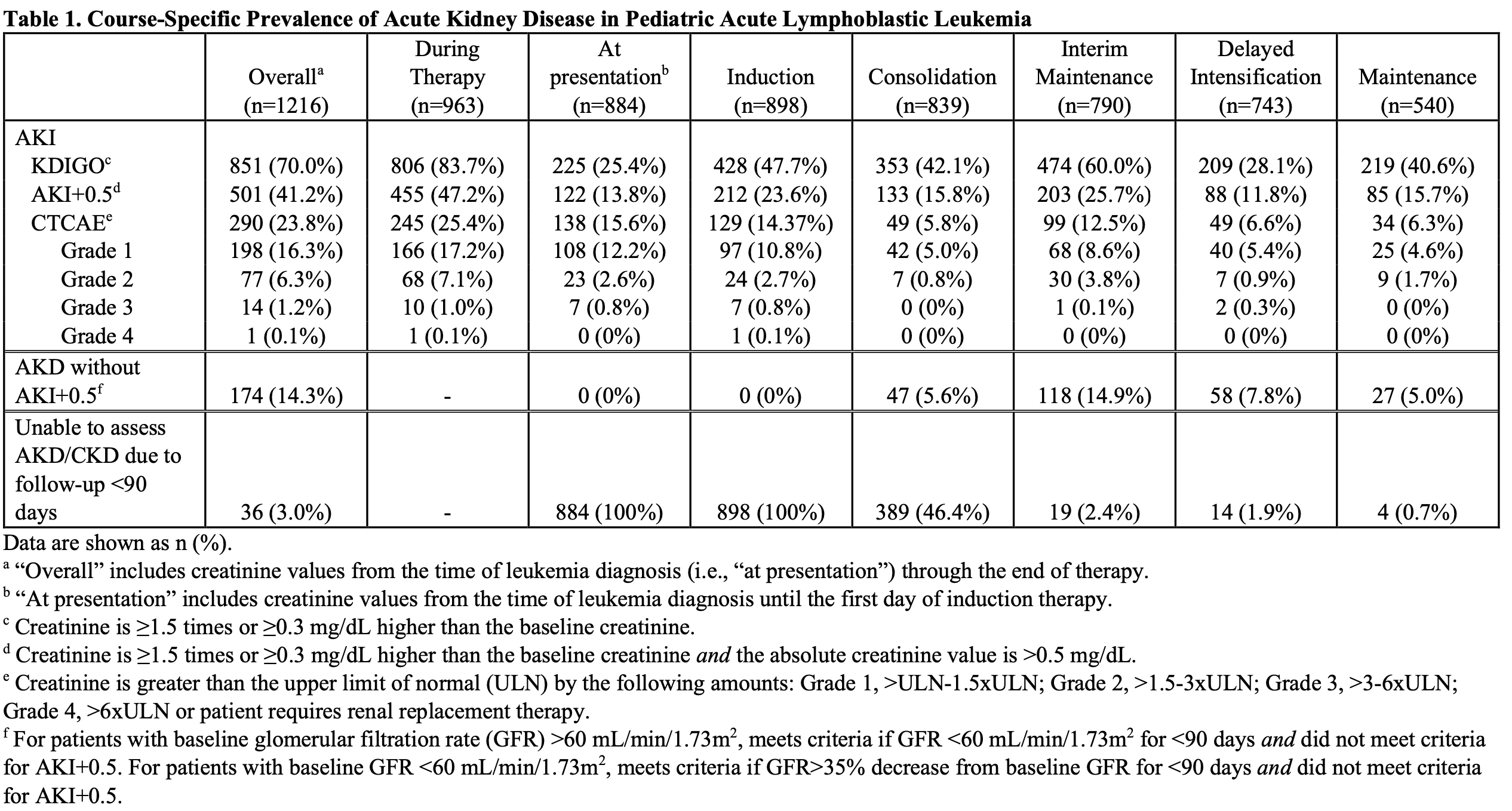
.png)
