Neurology: Neurodevelopment
Neonatal Neurology 5: Clinical
108 - Objective tools for early brain injury diagnosis and neurological prognosis in preterm infants based on aEEG assessment
Publication Number: 108.337
- CC
Cristina Cortés-Ledesma, MD (she/her/hers)
Neonatologist
Clinico San Carlos Hospital
Madrid, Madrid, Spain
Presenting Author(s)
Background:
Extreme preterm newborns (EPN) are at high risk for death or neurologic sequelae at discharge. Unfavorable short-term outcomes (USTO) are a well-known determinant for neurodevelopmental sequelae. There are no early reliable biomarkers predicting USTO. aEEG has emerged as a tool for EPN neuromonitoring, with increasing studies reporting on its predictive value. However, correct aEEG assessment is subjective and expertise-based, resulting in heterogenous results. As a result, the use of aEEG as a standard preterm monitoring is often discouraged.
Objective:
To obtain objective and practical tools based on aEEG to predict USTO in EPN
Design/Methods:
Infants born before 27 weeks GA admitted in our hospital between 2019 and 2022 were enrolled in a prospective, observational study (ethics committee approval: 20/772-E).
aEEG assessment: aEEG was recorded over the first 4 days of life (DOL) and then weekly until 4 weeks of life. Tracings were assessed according to Burdjalov score. Interbrust interval was calculated. High activity percentage (HAP) was determined as percentage of time with low border of aEEG trace above 5mV.
Short term outcome assessment: Survival at discharge or neuroimaging at term normal or with grade I intraventricular hemorrhage was considered as good short-term outcome. Otherwise, it was considered as USTO.
Results:
51 patients were enrolled, 19/51 (37.3%) patients presented good outcome, and 32/51 (62.7%) USTO. Clinical data stratified by USTO are shown in Tbl 1.
aEEG results: Burjdalov score as well as HAP increased earlier in normal outcome as compared to abnormal. Both presented high sensibility and specificity to predict USTO when analyzed at day 4 of life. The absence of rise of the HAP in the first four days of live is associated with USTO with high sensibility and positive predictive value. (Fig.1).
Among infants with USTO, administration of sedatives or time of diagnosis of structural brain damage (already at 4 DOL, or later) did not affect the predictive value of aEEG parameter (Fig.2)
Conclusion(s): HAP is described as an easy and objective tool to predict outcome using aEEG with very promising results. We found differences in aEEG parameters between infants with normal an abnormal outcome using the Burdjalov score, as well as the HAP, being the 4 DOL the better moment to predict outcome. The lack of increased of the HAP in the first four DOL is also associated with USTO. Sedation or timing of structural damage diagnosis did not affect the predictive value of aEEG. This adds prognostic value to aEEG compared to ultrasound alone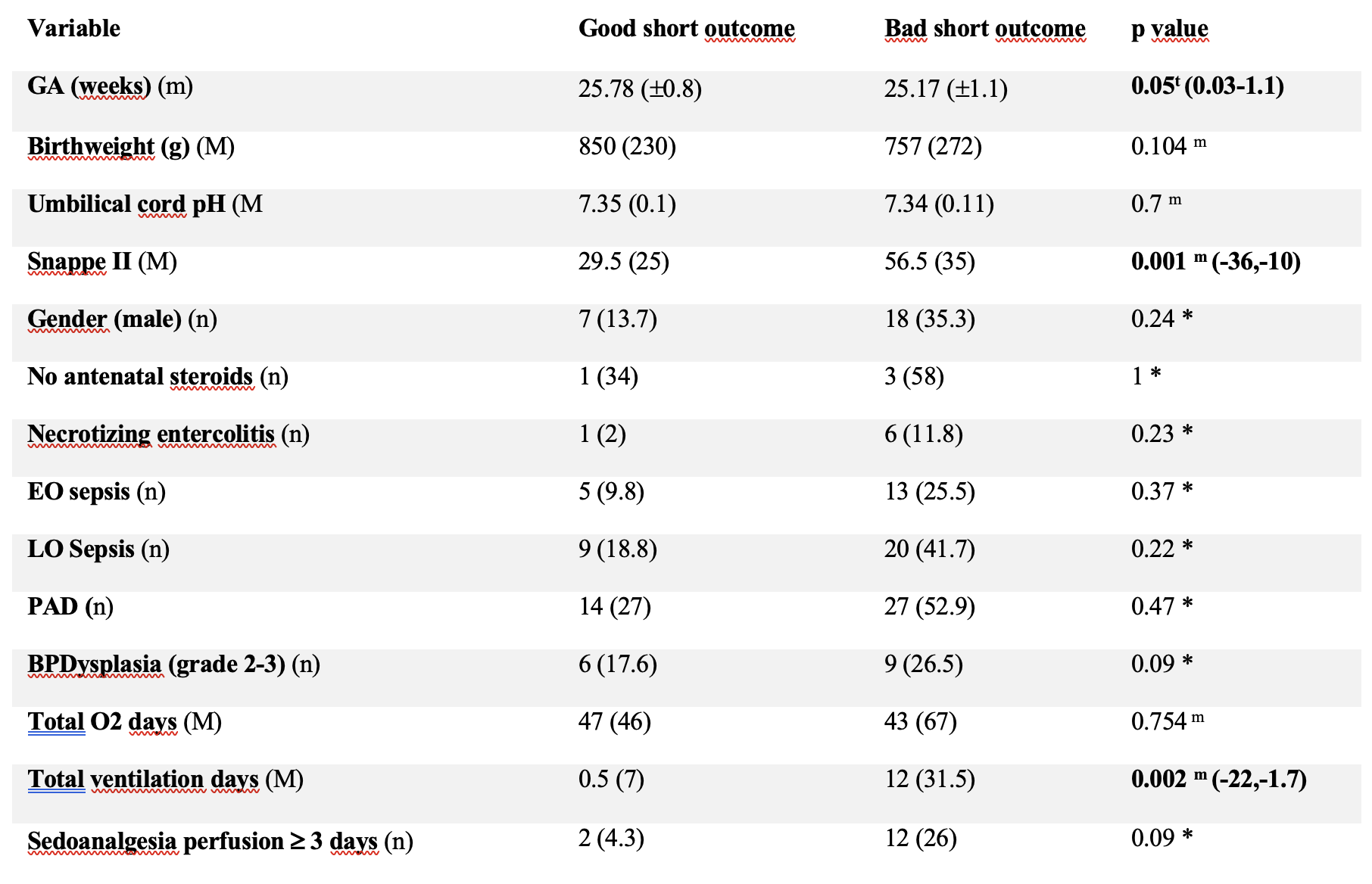
figure 1.2.JPEG
figure 2.1.JPEG
