Nephrology: Clinical
Nephrology 6: Glomerular/Clinical and Basic Science
62 - Histopathology Findings and Outcomes of Non-Nephrotic Range Proteinuria in Adults and Children
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 62
Publication Number: 62.351
Publication Number: 62.351
Ai Itoku, Children's Hospital at Montefiore, Long Island City, NY, United States; Lihong Bu, Mayo Clinic College of Medicine and Science, Rochester, MN, United States; Frederick J. Kaskel, lbert Einstein College of Medicine, Bronx, NY, United States; James M. Pullman, Albert Einstein College of Medicine, Bronx, NY, United States; Yujie Wang, University of Michigan Medical School, Ann Arbor, MI, United States; Kimberly J. Reidy, Children's Hospital at Montefiore, Bronxville, NY, United States

Ai Itoku, MD (she/her/hers)
Pediatric Nephrology Fellow
Children's Hospital at Montefiore
Flushing Hospital Medical Center
Long Island City, New York, United States
Presenting Author(s)
Background: While there are clinical practice recommendations for nephrotic syndrome, the approach to diagnosis and management of non-nephrotic range proteinuria (NNP) is not well defined.
Objective: The goal of this study is to better understand histopathology findings associated with NNP in adults and children. We hypothesized that the histopathologic diagnoses differ between subjects with NNP compared to nephrotic syndrome and between children vs. adults with NNP.
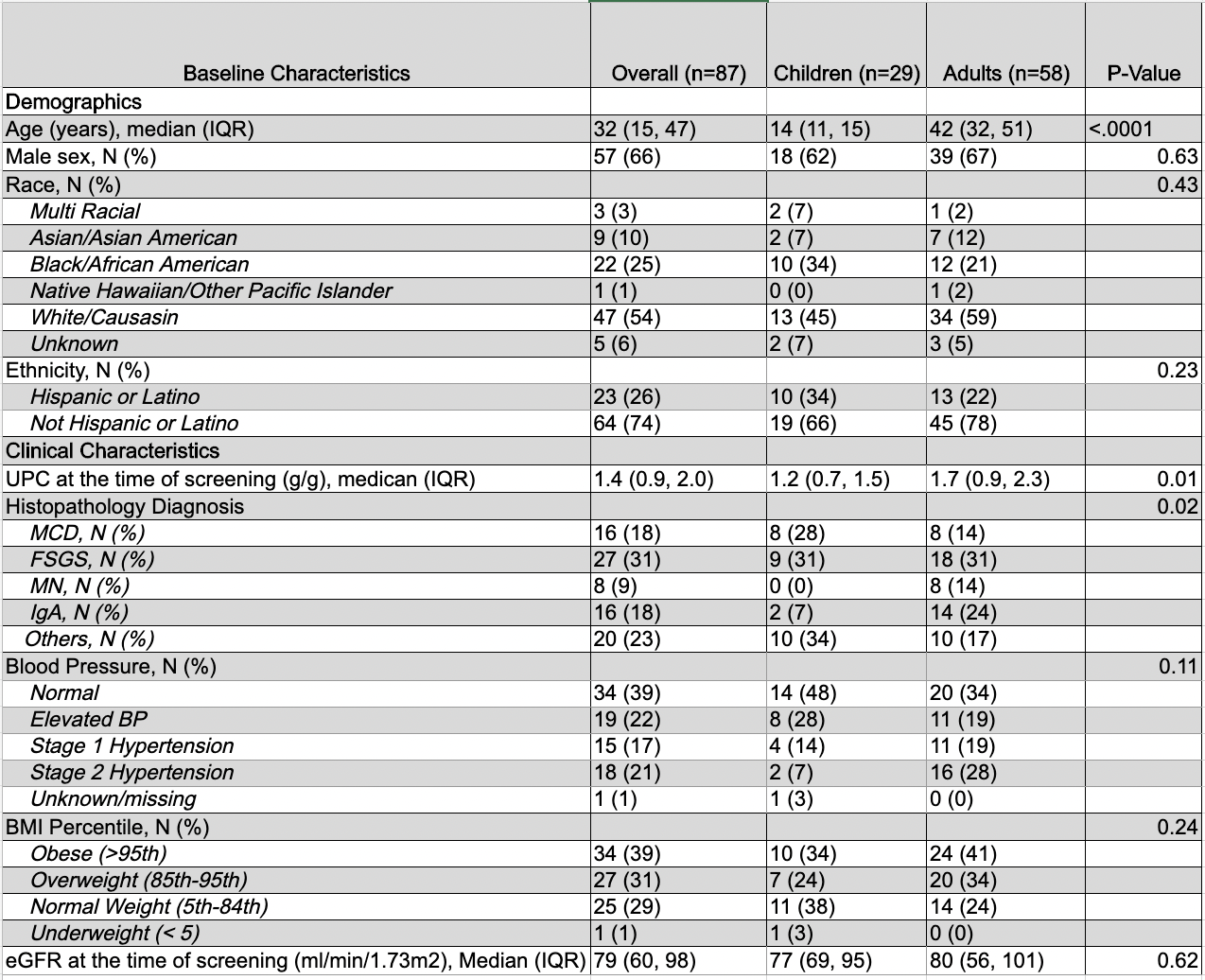
Design/Methods: We performed a secondary analysis of the Nephrotic Syndrome Study Network (NEPTUNE) study. NNP was defined as urine protein creatinine ratio ≥ 0.3 g/g but less than 3 g/g (adults) or 2 g/g (children). We included the subjects with NNP that had never received treatment prior to enrollment and examined histopathologic diagnoses and baseline demographic data. Continuous baseline variables were expressed as medians with interquartile ranges (IQRs) and categorical variables were expressed as frequencies (n) and percentages. Student T-test and Mann-Whitney U test were used when appropriate to compare continuous variables and Chi-square test or Fisher’s exact tests were used when appropriate to compare categorical variables.
Results: Total 58 adult and 29 pediatric participants were eligible for study inclusion. Histopathologic diagnoses differed between adult and pediatric participants with NNP (p=0.02). Of adult participants, 18/58 (31%) had Focal Segmental Glomerulosclerosis (FSGS), 14/58 (24%) had IgA Nephropathy, 10/58 (17%) had Other, and 8/58 (14%) had Minimal Change Disease (MCD) and Membranous Nephropathy (MS). Of pediatric participants, 10/29 (34%) had Other, 9/29 (31%) had FSGS, and 8/29 (28%) had MCD. At baseline (Table), 66% (38/58) adult and 49% (14/29) pediatric participants had either elevated blood pressure, stage 1 or stage 2 hypertension. Most adult (44/58, 75%) and pediatric (17/29, 58%) participants with NNP were classified as overweight or obese. Median baseline eGFR was 80 [IQR 56, 101] and 77 [IQR 69, 95] ml/min/1.73m2 and median eGFR decline was -1.7 [IQR -4.8, 2.0] and -2.3 [IQR -5.3, 3.3] ml/min/year in adults and children, respectively.
Conclusion(s): Histopathologic diagnoses differed in adults vs. children with NNP. There were high rates of hypertension and overweight/obesity at baseline. In addition, 17 % of adults were classified as “Other” and this was the most common histopathology classification in children. In ongoing studies, we are analyzing the detailed digital pathology data and longitudinal outcomes in this cohort. These studies may provide valuable information regarding NNP evaluation and management.