Global Neonatal & Children's Health
Global Neonatal & Children's Health 2
636 - Feasibility of Pediatric Acute Care Education’s Essential Newborn Care: An Adaptive E-Learning Environment to Improve Provider Proficiency
Publication Number: 636.316

Peter Andrew Meaney, MD MPH (he/him/his)
Clinical Professor
Stanford University School of Medicine
Menlo Park, California, United States
Presenting Author(s)
Background: Pediatric Acute Care Education (PACE) is an adaptive e-learning environment developed to improve healthcare provider knowledge of Tanzanian national guidelines for newborn and child acute care.
Objective: To determine feasibility of PACE’s adaptive Essential Newborn Care (aENC) modules at four facilities in Mwanza, Tanzania.
Design/Methods:
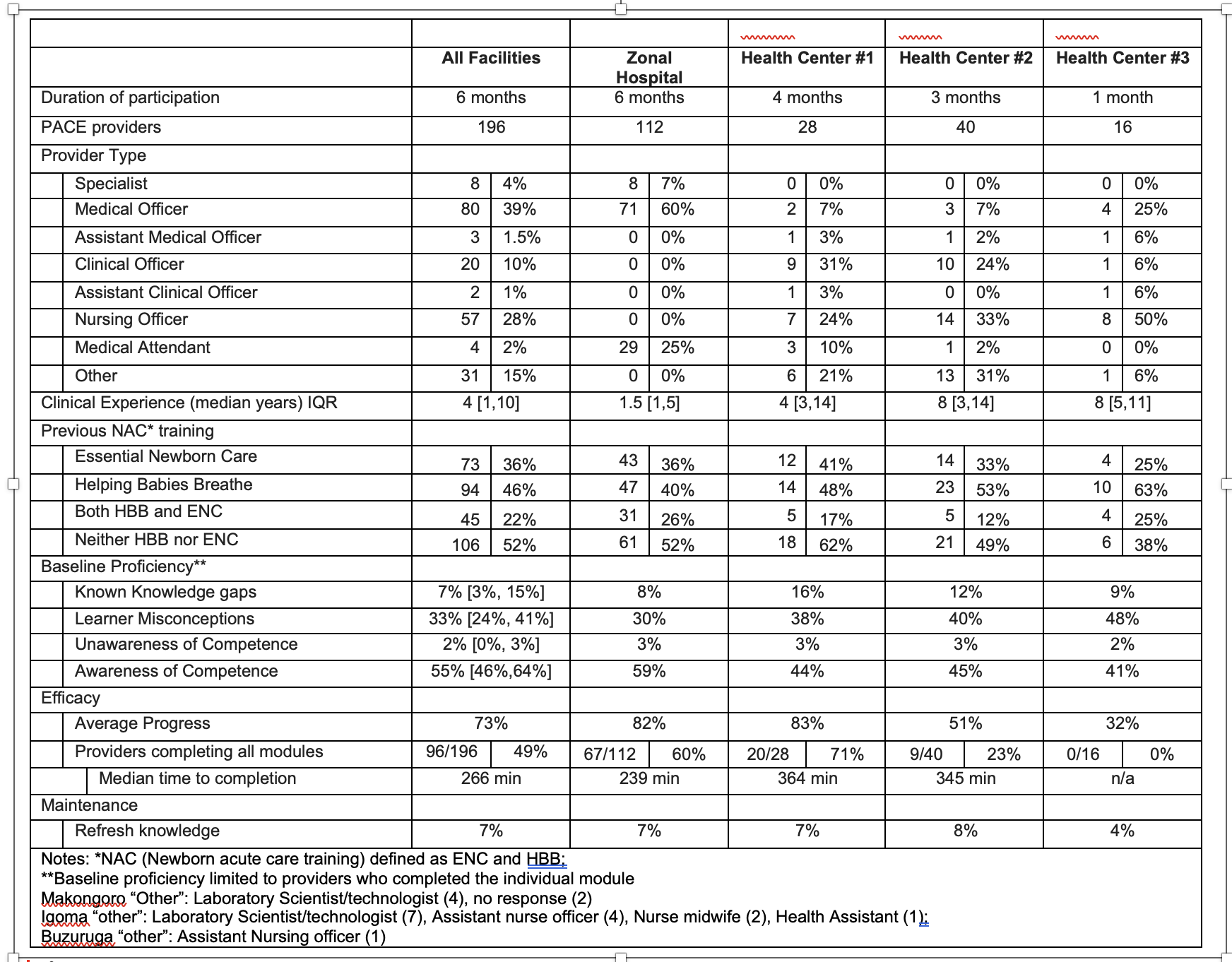
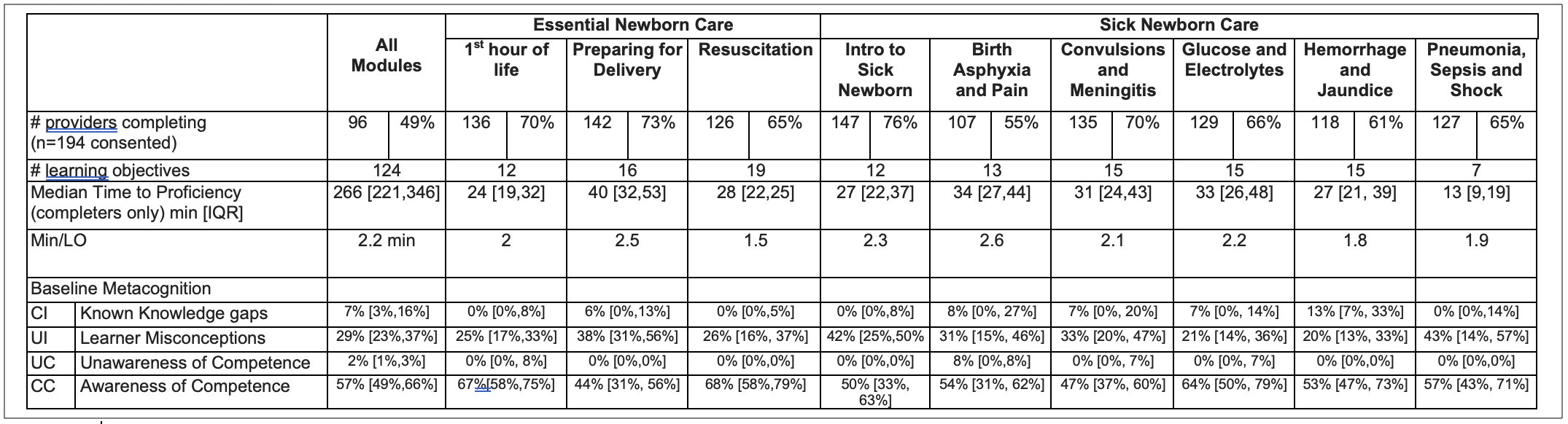
Observational cohort. We defined feasibility using RE-AIM, an established framework to assist translating research into implementation. Implementation feasibility was defined a-priori as: 1) Reach: >75% of eligible providers participating, 2) Efficacy: and increase in conscious competence >30%, Implementation: > 60% completed all initial learning assignments, 3) Adoption: all facilities; 4) Individual maintenance: >60% providers complete refresh assignments. Using Howell’s conscious-competence model, we defined efficacy as percent change of conscious competence from baseline. We reported facility and provider characteristics. We also reported median time to complete each module.
Results: 196 providers of all types participated from 4 facilities. 52% of providers had never received any newborn training and had median experience of 4 years [1,10].196/231(85%) of eligible providers participated in aENC with 96 (49%) completing all 9 modules. Median provider progress was 71% [36, 83%]. Median conscious competence increased 41% [39, 46%] from baseline and learner misconception decreased 29% [23,37%], representing 70% of baseline competence gaps. All facilities adopted aENC (n=4), no deviations from protocol were reported. No provider completed all refresh assignments and average progress was 7% [4%, 8%]. Median time to complete aENC was 266min [221,346].
Conclusion(s): aENC met all feasibility criteria of reach, efficacy, adoption, but not maintenance. PACE increased the reach of newborn acute care training to a heterogeneous, experienced workforce. Strategy revisions should target intrinsic and extrinsic motivators for refresher assignment completion. Correcting misconceptions, rather than new learning represents most of the proficiency gaps of providers..png)