Global Neonatal & Children's Health
Global Neonatal & Children's Health 1
622 - Making Every Newborn Resuscitation A Learning Event: Establishing a Newborn Resuscitation Registry in the Democratic Republic of the Congo
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 622
Publication Number: 622.315
Publication Number: 622.315
Amy Mackay, University of North Carolina at Chapel Hill School of Medicine, Durham, NC, United States; Daniel Ishoso, Kinshasa School of Public Health, Kinshasa, Kinshasa, Congo, (Congo – Kinshasa); Eric Musalu. Mafuta, Ecole de Santé Publique de Kinshasa, Kinshasa, Kinshasa, Congo, (Congo – Kinshasa); Melissa Bauserman, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Carl Bose, University of North Carolina at Chapel Hill School of Medicine, Pittsboro, NC, United States; Sara Brunner, Laerdal Medical AS, Stavanger, Rogaland, Norway; Joar Eilevstjønn, Laerdal Medical, Sandnes, Rogaland, Norway; Helge Myklebust, Laerdal Medical, STAVANGER, Rogaland, Norway; Jackie Patterson, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States

Amy Mackay, MD (she/her/hers)
Neonatal-Perinatal Fellow
The University of North Carolina at Chapel Hill
Durham, North Carolina, United States
Presenting Author(s)
Background: Each year, one million newborns die in the first 24 hours after birth. Most of these deaths occur in low- and middle-income countries (LMICs). Neonatal deaths in the first 24 hours are predominately caused by intrapartum events, resulting in failure to breathe at birth. One third of these intrapartum-related deaths could be averted with basic resuscitation. To improve basic resuscitation, a detailed record of provider actions during resuscitation is essential. However, obtaining these data is challenging in most LMICs because medical records do not typically provide sufficient granularity.
Objective: To establish a detailed newborn resuscitation registry in the Democratic Republic of the Congo (DRC).
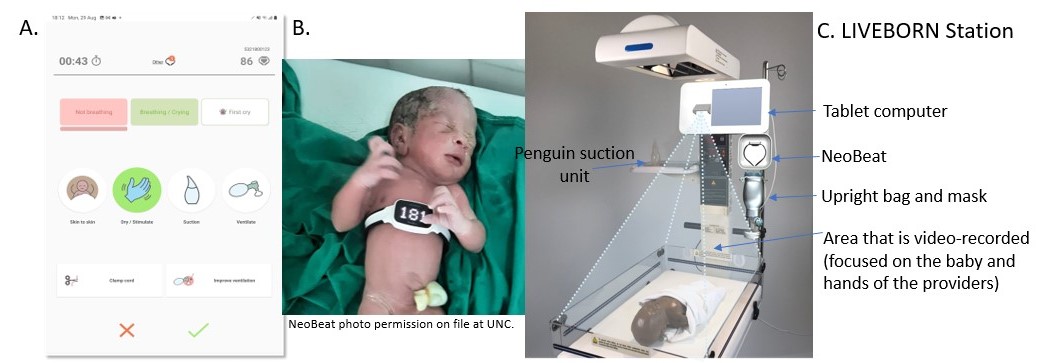
Design/Methods: We established a resuscitation registry at two health facilities in Kinshasa, DRC. Study nurses abstract clinical data of all in-born neonates from the delivery register using KoboToolbox, with a focus on known risk factors for failure to breathe at birth including low birth weight and prematurity, and vital status at discharge. In a convenient sample of ≥50% of deliveries, a cadre of trained observers (study nurses, midwives, and environmental health services staff) document provider actions and the newborn’s respiratory status during resuscitation using a mobile health application, LIVEBORN (Figure 1). In the subset of observed non-vigorous newborns (defined as not breathing by 30 seconds after birth), we stream continuous heart rate data to LIVEBORN using a heart rate meter, NeoBeat (Figure 1). LIVEBORN data (linked with NeoBeat data when applicable) are stored in a cloud-based server and analyzed with Matlab.
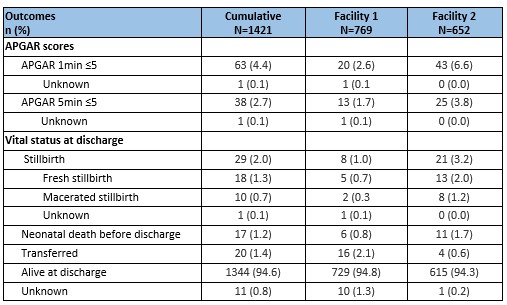
Results: From 9/1/22 to 12/1/22, we enrolled 1421 newborns. We abstracted medical record data on 100%; clinical data were reliably recorded in the medical record, except for meconium-stained fluid (94.9% unknown) and gestational age (2.2% unknown; Table 1); vital status at discharge was missing for 0.8% (Table 2). We observed 836 newborns with LIVEBORN (58.8%). Among the 109 observed non-vigorous newborns, we integrated NeoBeat heart rate data on 17.
Conclusion(s): Establishing a newborn resuscitation registry using medical record abstraction, a mobile health application, and an electronic heart rate meter is feasible in a low-resource setting. Integration of heart rate data could be improved with more consistent use of NeoBeat by providers. In January 2023, we will add videorecording of resuscitation care to our registry using the LIVEBORN station (Figure 1). This resuscitation registry is an essential first step to evaluate strategies for improving resuscitation care.
.jpg)