Hematology/Oncology
Hematology/Oncology 1
150 - Epidemiology, Trends, and Healthcare Burden of Post-Transplant Lymphoproliferative Disorder among Pediatric Recipients of Solid Organ or Hematopoietic Stem Cell Transplant
Publication Number: 150.22

Thrisha Kalpatthi (she/her/hers)
High School Student
UPMC Childrens Hospital of Pittsburgh
Mars, Pennsylvania, United States
Presenting Author(s)
Background:
Post-transplant lymphoproliferative disorder (PTLD) is the most common malignancy occurring after hematopoietic stem cell transplant (HSCT) or solid organ transplant (SOT) secondary to immunosuppression or oncogenic viral infections. The healthcare burden of HSCT or SOT is substantial and the occurrence of PTLD presumably incurs additional burden among these patients. Data describing the trends and healthcare burden of PTLD after pediatric patients receive HSCT/SOT is limited.
Objective: To describe the incidence, annual trends, mortality, and healthcare resource utilization of PTLD
among hospitalized pediatric patients who received HSCT or SOT.
Design/Methods:
We used the Pediatric Health Information System (PHIS), an administrative database of free-standing children's hospitals in the US. Using ICD-9 and ICD-10 procedure and diagnosis codes, patients under the age of 21 who underwent HSCT or SOT at one of the 49 PHIS hospitals from 2008-2021 were identified. The PHIS database provides an encrypted patient medical record number, which allowed for better visualization of the patient's hospitalizations trend over 11 years. We abstracted data on transplant type, demographics, medications, mortality, resource utilization, and costs. All statistical analyses were performed using Stata version 17.
Results:
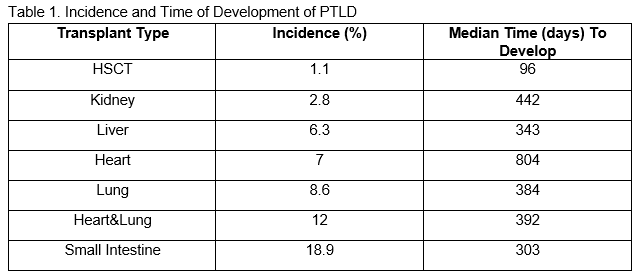
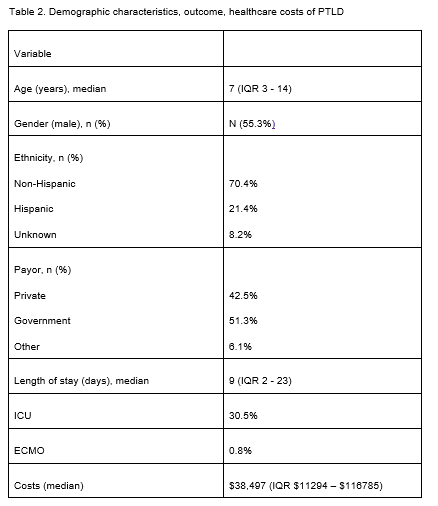
A total of 31,228 unique pediatric patients who received HSCT or SOT were identified. Among these 1012 (3.2%) children were identified to have the diagnosis of PTLD, with mortality of 14.1%. The incidence of PTLD and the median time (days) to develop PTLD by transplant type are shown in Table 1. Overall, the trend of PTLD diagnosis was increasing in our cohort over the years (Figure 1). The demographic characteristics and outcomes of these children with PTLD are shown in Table 2. Interestingly, Rituximab during the initial transplant encounter was associated with increased risk of mortality in patients who developed PTLD following HSCT (p< 0.001), liver (p=0.017) and heart SOT (p=0.022). Multivariate analysis including age, gender, ethnicity, transplant type, insurance payor, urban designation, cyclophosphamide and rituximab use in index PTLD encounter and year of PTLD demonstrated use of cyclophosphamide was associated with increased mortality (OR 8.52 (4.09-17.73).
Conclusion(s):
Our data shows increasing incidence of PTLD following HSCT or SOT in pediatric patients over the years. Use of rituximab during initial immunosuppressive regimen may be linked to increased mortality in patients who developed PTLD. Further studies are needed to explore this association. .png)