Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 2
660 - Antibiotic Use Among Surgical Patients in the Neonatal Intensive Care Unit (NICU): The NO-More-AntibioticS and Resistance in Surgery (NO-MAS-R-S) Study
Publication Number: 660.241

Pavel Prusakov, PharmD (he/him/his)
NICU/ASP Clinical Pharmacist
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background:
Although antibiotic exposure among infants in the NICU is associated with short- and long-term adverse effects, the burden of antibiotic use in neonatal surgical patients has not been well described. The pediatric surgical team at Nationwide Children’s Hospital (NCH) provides all surgical consultations for central Ohio in the level 4 outborn referral NICU at NCH.
Objective: Our objective was to quantify the total use of antibiotics in surgical NICU patients and thus identify antimicrobial stewardship opportunities.
Design/Methods:
This was a prospective observational study of all infants in the NCH NICU who underwent pediatric surgical evaluation and received antibiotic therapy from 1/3/2022 to 6/30/2022. The pediatric surgery fellow informed the neonatal clinical pharmacist about all consultations and provided qualitative data on antibiotic prescribing (diagnosis, indication and reasoning for antibiotic selection, dosing, and duration) using a set questionnaire. Pertinent demographic maternal/infant data were obtained from the electronic health records.
Results:
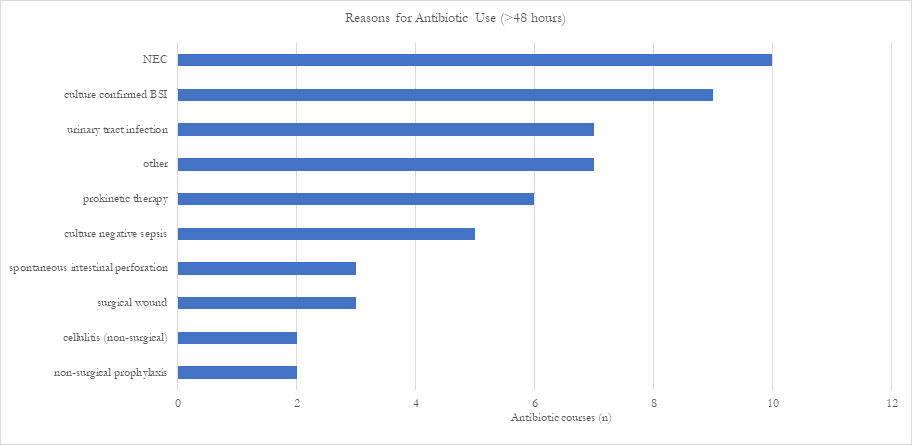
During the 6-month study period, 94 infants (mean ± SD gestational age, 34 weeks ±5.2; birthweight, 2216 ±1079 g) underwent surgical evaluation at a median postnatal age of 2 days (IQR, 1-15 d). 55 (57%) infants were male; 21 (22%) had antibiotic exposure for >48 hours before surgical consultation. Of the 94 infants, 74 (79%) had at least one antimicrobial course although only 48 (51%) had any surgical procedure performed. Indications for antibiotic use are provided in Figure 1 with necrotizing enterocolitis the most frequent. Surgical site cultures were done in only 3 infants. Of the 48 infants who underwent surgery, the most commonly used antibiotics were cefazolin (32%), ampicillin-sulbactam (23%), piperacillin-tazobactam (12%), and cefoxitin (10%). Cefazolin was used primarily for surgical prophylaxis for an average of 2 doses ±1.8. Of patients receiving antimicrobial therapy, only 4 of 70 infants were colonized with methicillin-resistant Staphylococcus aureus. The most frequent blood isolate was E. coli (n=4). Overall mortality was 6% (n=6). The only infection-related death was in an infant who died of sepsis due to Pseudomonas aeruginosa, unrelated to surgery.
Conclusion(s):
Antibiotics were utilized in the majority of infants who had a surgical consultation. Several stewardship opportunities were identified including reduction in cefazolin use pre- and post-operatively and use of an anti-staphylococcal beta-lactam agent as first-line therapy for non-purulent cellulitis.
*Funded by a research grant from Merck