Endocrinology: QI/Practice
Endocrinology 2
197 - Managing Diabetic Ketoacidosis in a Moderate Care Unit: A Quality Improvement Initiative
Publication Number: 197.214
- AR
Alexander J. Rogers, MD, FAAP (he/him/his)
Associate Professor of Emergency Medicine
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background:
For improved care of our pediatric diabetic ketoacidosis (DKA) patients, our tertiary care pediatric hospital implemented an insulin drip and 2-bag system of dextrose and fluid delivery. This acute and intensive care condition has been managed either in the emergency department (ED) or the pediatric intensive care unit (PICU) at our institution. However, limitations of general pediatric beds have resulted in longer wait times in both the ED and PICU, delays in starting new-onset diabetes education for families, and thus longer hospitalization times.
Objective:
Our objective was to establish a moderate care unit on the general pediatrics floor to care for patients with mild-moderate DKA on an insulin drip with 2-bag fluid delivery method. We hypothesized that this shift in our care model will shorten overall length-of-stay (LOS) in the hospital.
Design/Methods:
We characterized “mild-moderate DKA” as patients with a pH on a VBG of ³ 7.2 and a serum bicarbonate ³ 13. We included children ³ 5 years old. Once patients met these criteria, they were transitioned from either the ED or PICU to moderate care, making them eligible for a general pediatrics bed.
Prior to implementation, we used quality improvement (QI) methods to map out the current state workflow and the proposed moderate care workflow. Interdisciplinary team members from pediatric endocrinology, hospital medicine, emergency department, and nursing reviewed and revised the proposed workflow. We created educational materials for pediatric hospitalists, residents, and nurses. We also developed detailed protocols for both residents and pediatric hospitalists who oversee overnight care of these moderate care DKA patients.
Results:
Over the past 6 months (May 2022 – November 2022), 26% of DKA patients (n=12) were cared for with this new initiative. When compared to DKA patients treated during the prior year, LOS did not show a consistent month-to-month difference (Fig 1). However, the overall hospital LOS after the implementation of the moderate care unit was shorter compared to before (Fig 2). Of note, no untoward events occurred with need to reinstate an insulin drip.
Conclusion(s):
Through this QI intervention we found that mild-moderate DKA can be successfully cared for in a moderate care setting and doing so shortens the overall LOS for hospitalized patients with diabetes who present in DKA. Our project is still in its early phases with potential to further explore its impact on patient flow in the hospital. Shorter LOS in the hospital can overall help with inpatient patient burden and have positive financial implications for the hospital.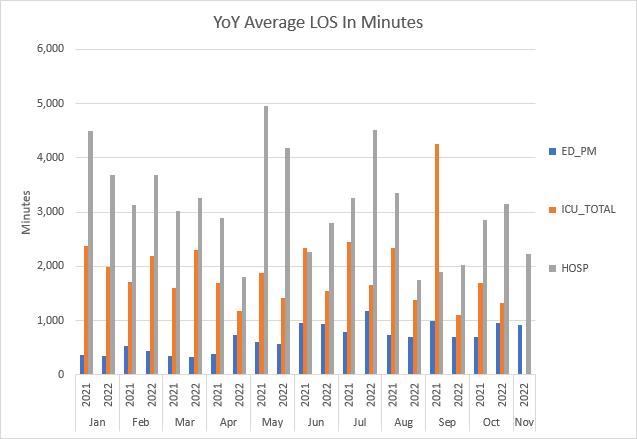
.png)
