Neonatal Neurology: Clinical Research
Neonatal Neurology 6: Clinical 6
135 - Transcatheter closure vs. Surgical Ligation of the Patent Ductus Arteriosus: Comparison of Cognitive Outcomes of Preterm Infants at 2 years age
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 135
Publication Number: 135.338
Publication Number: 135.338
Saima Sharif, Children's Hospital of Michigan, Dearborn, MI, United States; Girija Natarajan, Children's Hospital of Michigan, Detroit, MI, United States

Saima Sharif, MD (she/her/hers)
Fellow
Children's Hospital of Michigan
Dearborn, Michigan, United States
Presenting Author(s)
Background: The traditional treatment of preterm infants with patent ductus arteriosus (PDA) in whom medical therapy has failed or is contraindicated is surgical ligation (SL). In 2019, the FDA approved a device for transcatheter closure (CC) of PDA; however, comparative long-term outcomes are lacking.
Objective: To determine if preterm infants with PDA who underwent CC compared to SL had improved neurodevelopmental outcomes at 2 years age.
Design/Methods: This was a single-center prospective observational study of preterm (< 32 weeks gestational age-GA) infants who underwent CC vs. SL from Jan 2019 to Dec 2020. PDA closure modality was by parental choice. Clinical data were collected by electronic medical record review. At 2 years corrected age, the Parental Report of Cognitive Abilities revised (PARCA-R) was administered to parents and total composite (PRC) score, language [verbal developmental scale (VDS) range 0-100] and nonverbal cognitive scale (NVCS) [range 0-34] were obtained. The PARCA-R provides a norm-referenced, standardized assessment of cognitive and language development at 23-27 months of age. The primary outcome was cognitive impairment, defined as PRC < 50. Statistical analysis (SPSS 25.0) included t-test and chi-squared test and binary logistic regression to assess the association of cognitive impairment with GA, CC vs. SL, maternal education (high school vs higher level) and Grade 3 or 4 intraventricular hemorrhage (IVH).
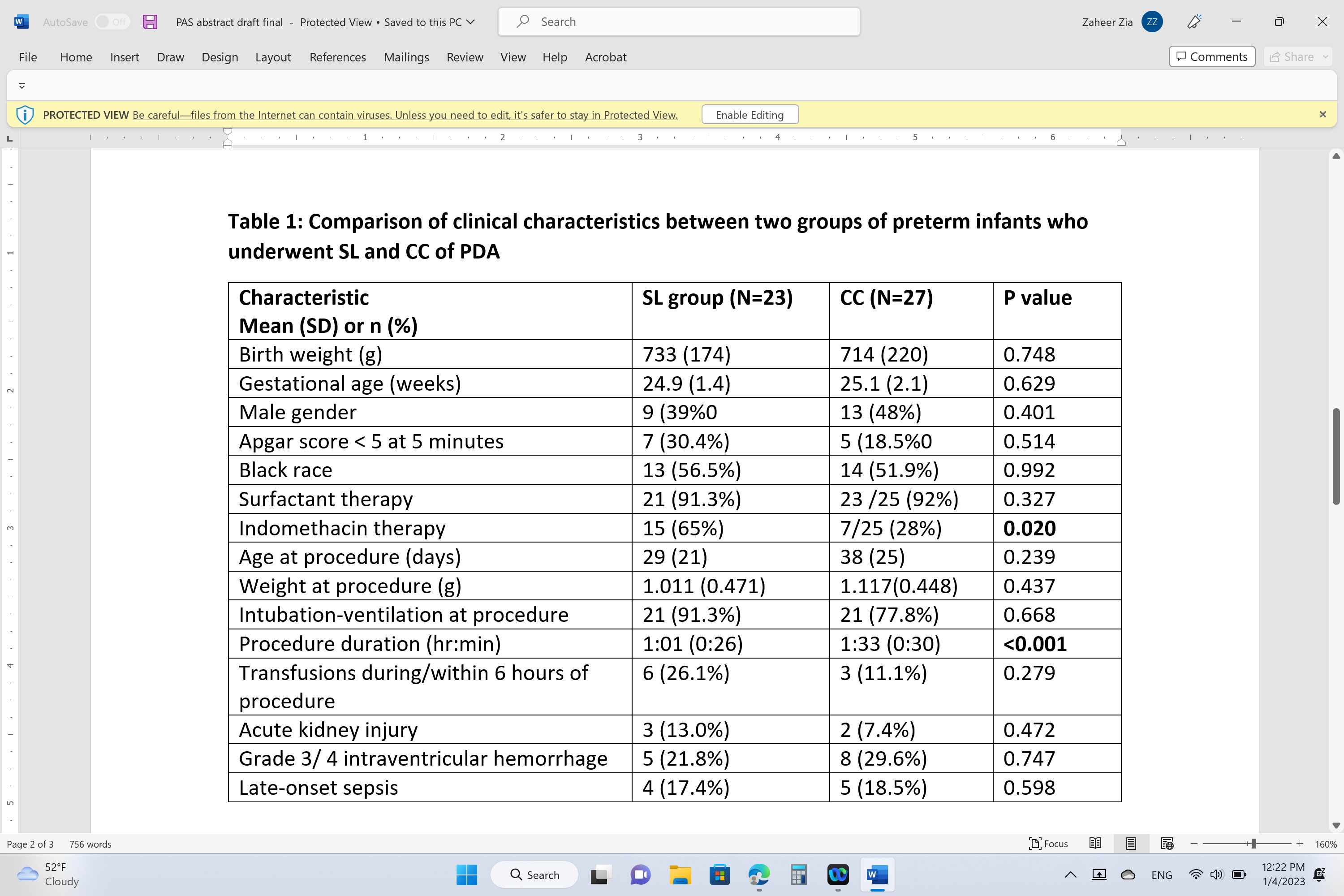
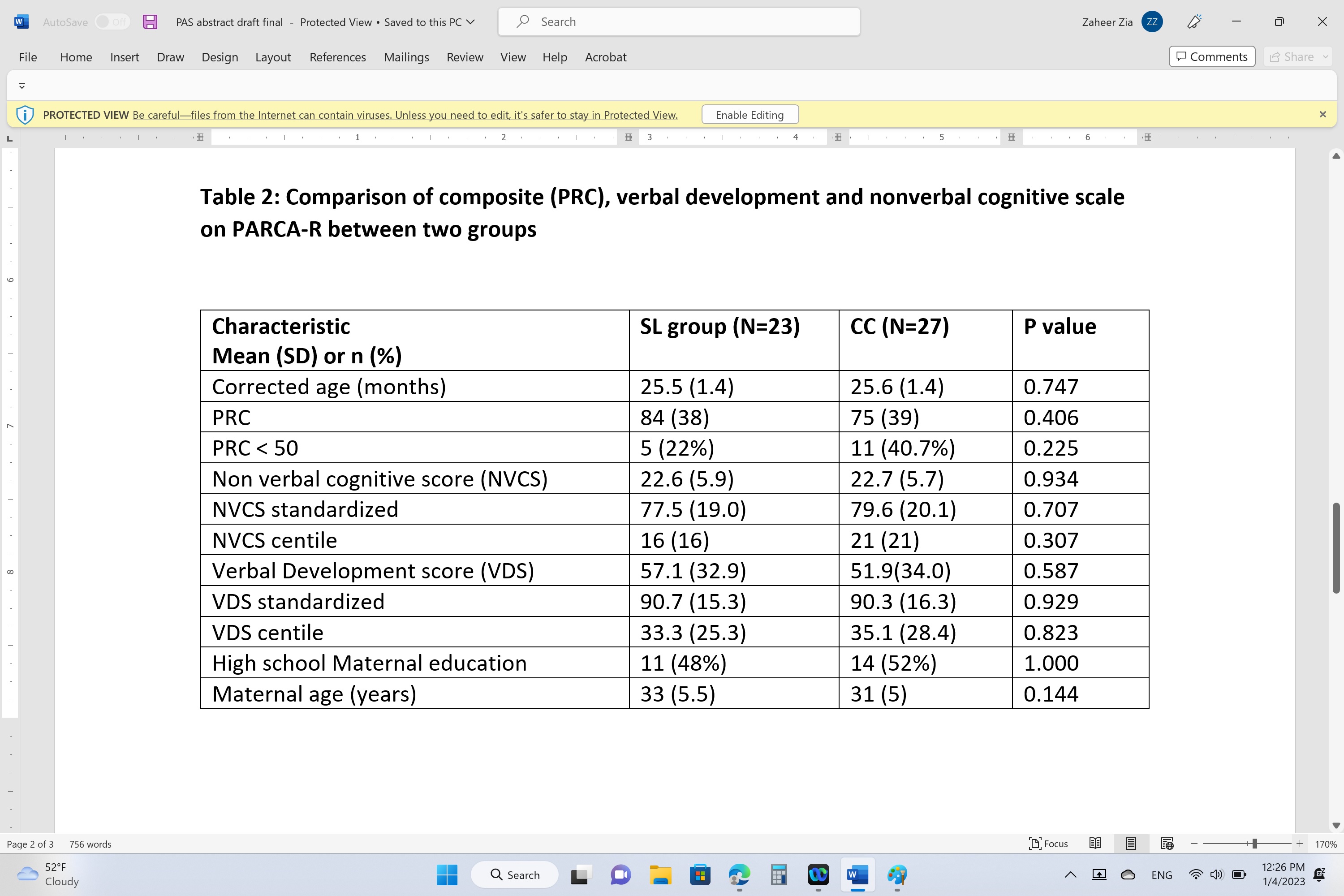
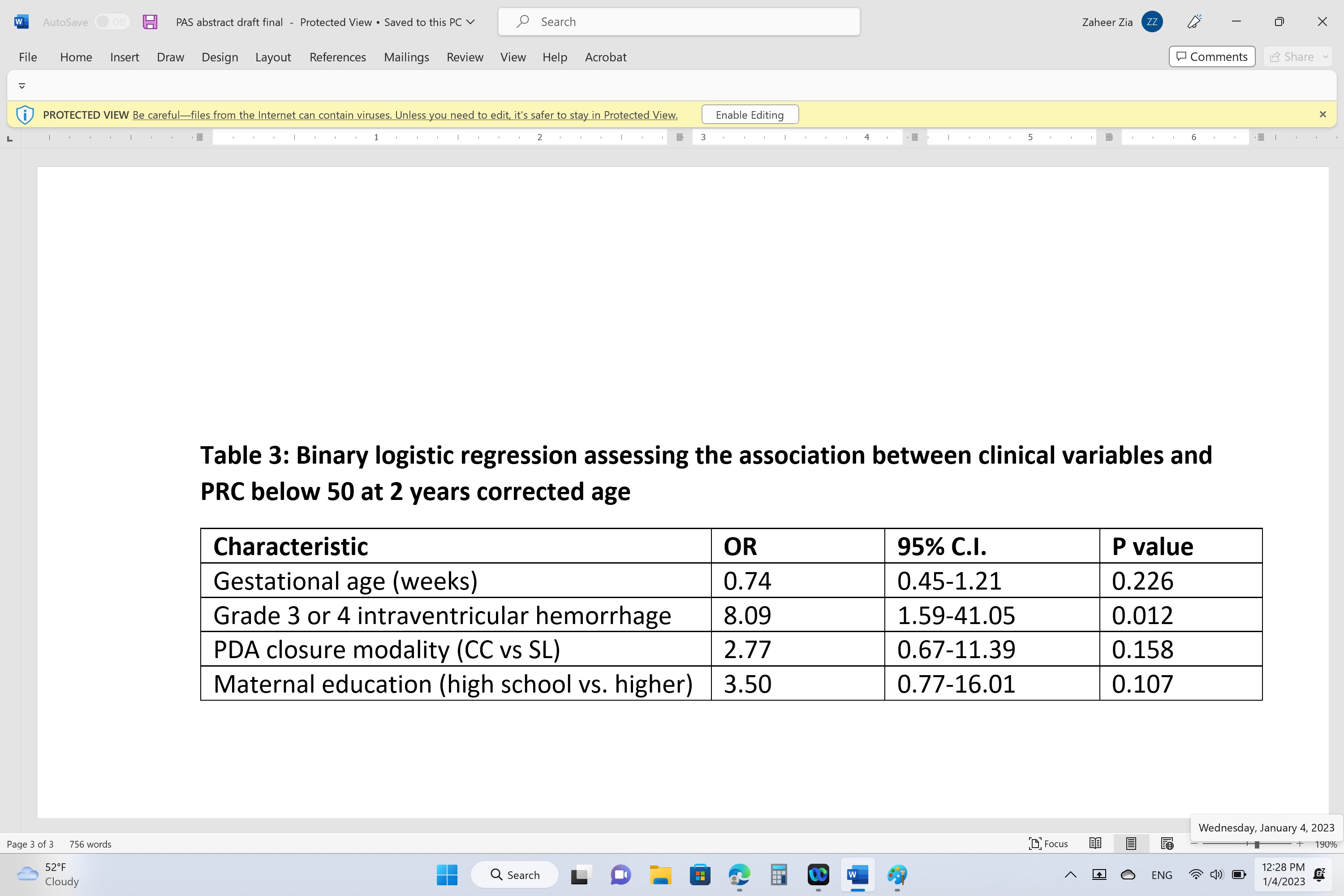
Results: Of the 77 infants who underwent PDA closure, 11 died, 16 parents did not respond; our cohort (n=50) comprised 23 in SL and 27 in CC group. Birth and clinical characteristics were comparable between the two groups except for a longer mean (SD) procedural duration and a less indomethacin therapy for CC [Table 1]. Table 2 is a comparison of PRC, VDS and NVCS scales between the two groups. The mean PRC in both groups were comparable at 84 and 75; SL group had 5 (22%) infants and the CC group had 11(41%) infants with PRC < 50 but the difference was not statistically significant. On regression analysis, only Grades 3 or 4 IVH [OR 8.09, 95% C.I. 1.54-41.05; p=0.012] was significantly predictive of PRC below 50; other assessed variables (GA, PDA closure modality, and maternal education) were not [Table 3].
Conclusion(s): We did not find statistically significant and clinically meaningful differences in cognitive or language outcomes at 24 months age between the SL and the CC groups, using a validated parental questionnaire. Further studies with larger sample size are warranted to determine if there is any smaller difference.