Emergency Medicine: All Areas
Emergency Medicine 6
354 - Hospital variability in psychotropic medication administration during emergency visits for children with mental and behavioral health conditions
Publication Number: 354.21

Ashley A. Foster, MD (she/her/hers)
Assistant Professor, Emergency Medicine
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background:
Emergency department (ED) utilization for pediatric mental and behavioral (MBH) conditions is increasing over time. While in the ED, this vulnerable population may be at risk of adverse events such as medication errors. Additionally, there is limited evidence to guide medication administration in children with acute MBH symptoms, often confining use to off-label administration. Although consensus guidelines exist for the treatment of acute agitation in the ED, there may be practice variation in ED psychotropic medication administration for children with MBH conditions.
Objective:
We aimed to describe types of psychotropic medications administered to youth in the ED with MBH conditions, assess changes in medication use over time, and explore variability in ED psychotropic medication administration across hospitals.
Design/Methods:
A cross-sectional study of ED encounters by children 3-21 years with primary MBH conditions at U.S. children’s hospitals using the Pediatric Health Information System from academic year 2013-2022. Psychotropic medications were categorized as psychotherapeutic, stimulants, anticonvulsants, antihistamines, antihypertensives, or other. To calculate changes in individual and cumulative use over time, we estimated logistic regression models with medication use as the dependent variable and time as the independent variable. Effect estimates were reported as odds ratios (OR) with 95% confidence intervals (CI).
Results:
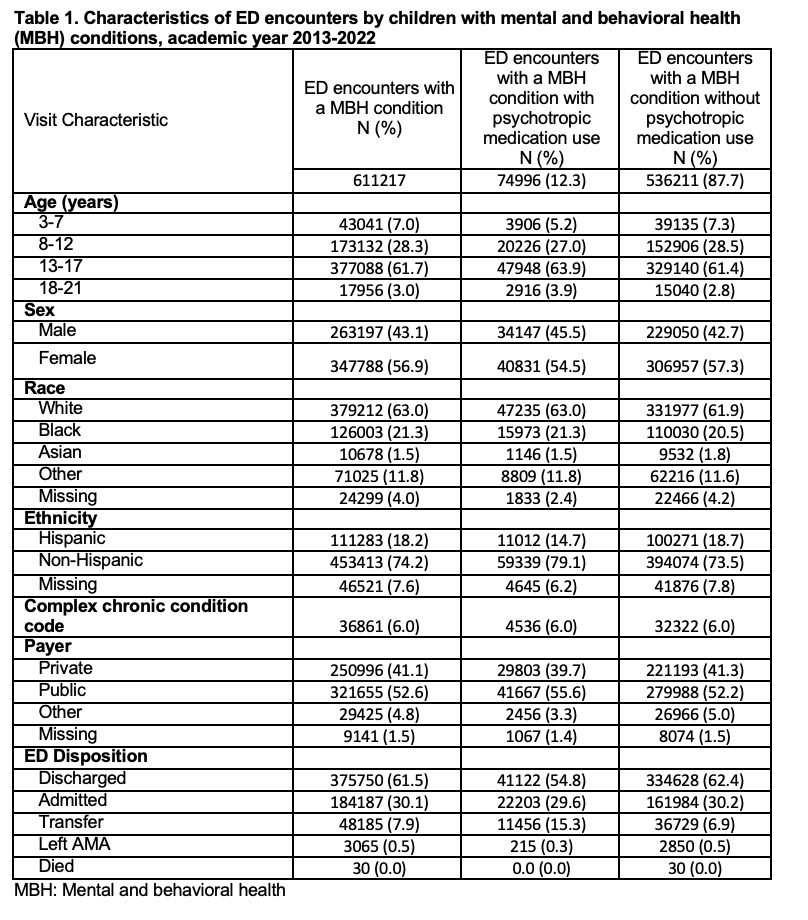
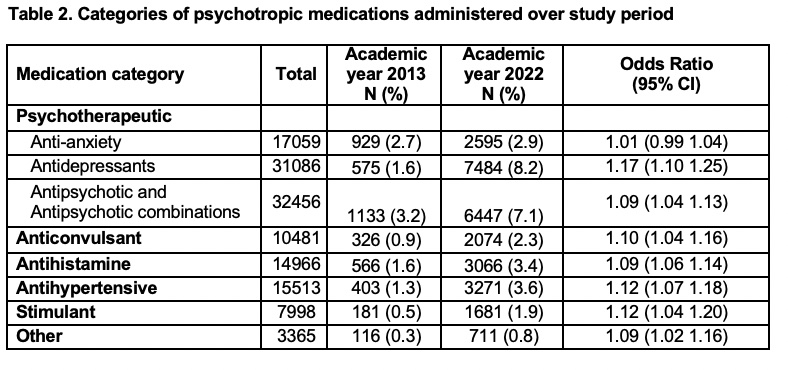
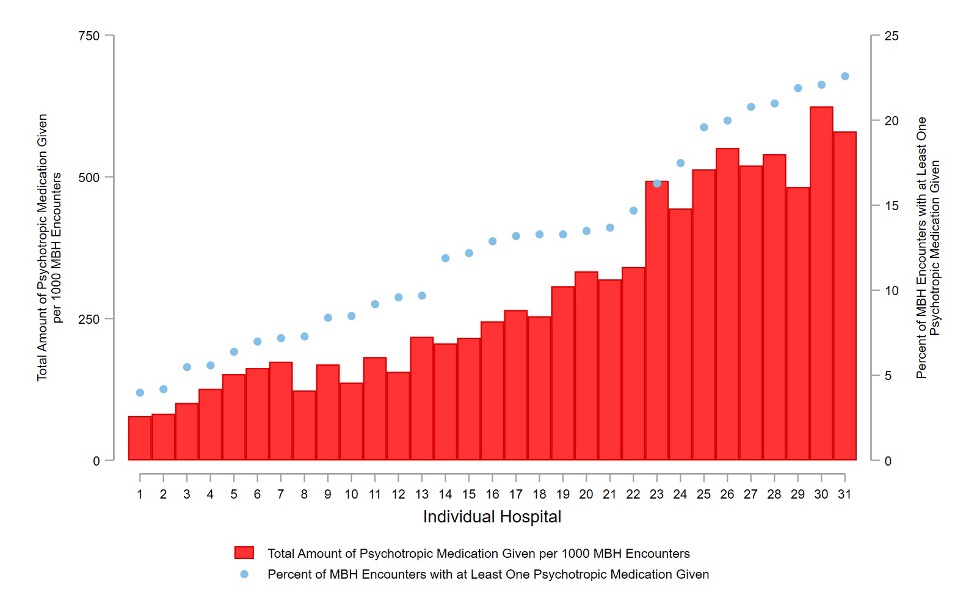
Of 611,217 encounteres with a MBH diagnosis, 12.3% had psychotropic medication administered in the ED (Table 1). Administration of all medication categories except for anti-anxiety medications increased significantly over time (Table 2). Administration of anti-depressant medications increased the most during the study period (OR 1.17; 95% CI 1.10-1.25). Among the 31 hospitals included, the number of psychotropic medications per 1000 MBH encounters varied from 330 to 8371, and the percent of MBH encounters with at least one psychotropic medication given ranged from 4% to 22.6% (Figure 1).
Conclusion(s):
Administration of psychotropic medications during MBH ED encounters by youth has increased over time, with considerable variation in use across children’s hospitals. These data reinforce the need for further study of ED management of children with MBH conditions and highlight an opportunity to standardize ED processes to enhance quality of care.