Mental Health
Mental Health 2
395 - Mental Health Supports in School: Pediatrician Perspectives and Policy Prescriptions for Improving Equitable Access and Service Reimbursement
Publication Number: 395.231
.jpg)
Ananya Tadikonda (she/her/hers)
Undergraduate Student
The University of North Carolina at Chapel Hill, Gillings School of Global Public Health
Boyds, Maryland, United States
Presenting Author(s)
Background:
With rising rates of youth mental illness, >60% receive no treatment, and minority and low income youth are disproportionately impacted. The AAP recommends depression screening for ages 12+; however, connecting youth to follow-up is often difficult. Schools are an underutilized equity-promoting setting for services with minimized transportation barriers. Youth are 6 times more likely to complete school-based vs community-based therapy, though reimbursement is often a barrier.
Objective: 1) Identify barriers and facilitators for pediatricians to screen for depression and develop follow-up plans and 2) Examine policies affecting reimbursement and access to behavioral health supports in schools.
Design/Methods:
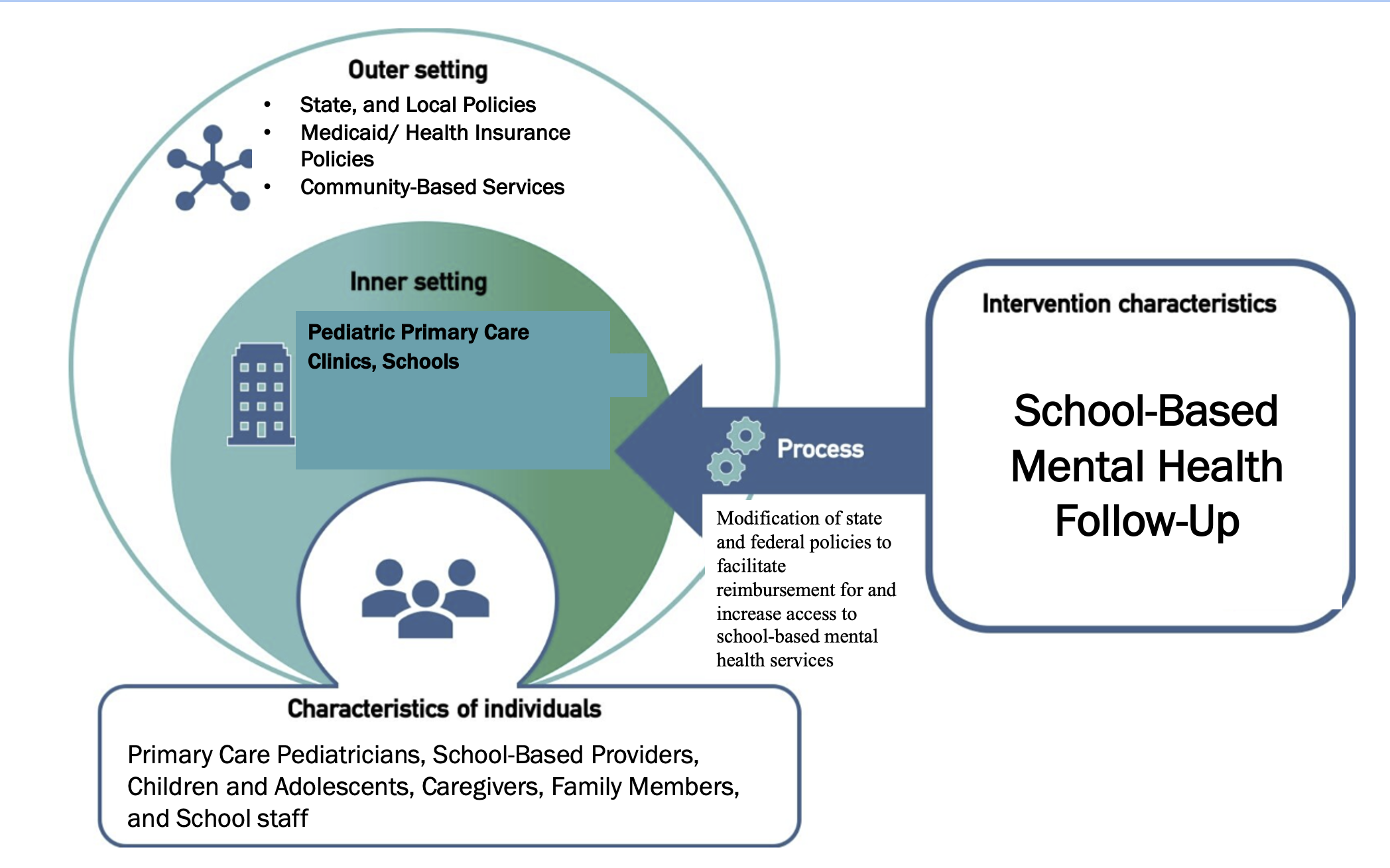
Using the Consolidated Framework for Implementation Research, we examined the internal context by analyzing 11 semi-structured interviews with pediatricians on screening for and managing depression. To investigate the external context, we reviewed Medicaid policies for school-based mental health services and related CMS guidance. Policy prescriptions are refined through qualitative interviews with leading field experts.
Results: Pediatricians identified fewer barriers to screening than in referring to services. Barriers to follow-up included inadequate mental health insurance coverage, overburdened mental health systems, and absence of language-concordant providers. Across states, 17 expanded Medicaid coverage in schools, and 48 reimburse for at least 1 type of behavioral health staff.
Based on our findings, the following are likely to improve access to mental health services in schools:
1. No wrong door approach: Provide opportunities for Medicaid enrollment and referral for care management through schools
2. Standardize coverage: Develop standardized school mental health benefits that are required in Medicaid contracts and recommended for private insurers, inclusive of preventive services (e.g., teaching mindfulness)
3. Reduce administrative burden: Offer centralized school health documentation systems and eliminate duplicative requirements; centralize school credentialing and billing across health plans
4. Increase reimbursement: For school-based mental health services, including through novel funding sources (e.g., tax revenue from marijuana sales in Colorado)
Conclusion(s): Strengthening behavioral health services in schools is an approach that pediatric providers could leverage for follow-up for children who screen positive for mental health issues. Policy changes that facilitate reimbursement of school-based mental health services can improve management and advance equity.