Neonatal Nephrology/AKI
Neonatal Nephrology/AKI 2
232 - Delayed cord clamping is associated with decreased estimated glomerular filtration at two-years in extremely premature neonates; a secondary Preterm Erythropoietin Neuroprotection Trial analysis
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 232
Publication Number: 232.243
Publication Number: 232.243
Namrata Todurkar, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Henry Zapata, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Jennifer R. Charlton, University of Virginia, Charlottesville, VA, United States; Tapas Kulkarni, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Ryan McAdams, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Michelle C. Starr, Indiana University School of Medicine, Indinapolis, IN, United States; Cherry Mammen, BC Children's Hospital, Vancouver, BC, Canada; Matthew Harer, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Kristen Favel, University of California, San Francisco, School of Medicine, San Francisco, CA, United States

Namrata Todurkar, MBBS, MD, DNB, FNNF, FNPM (she/her/hers)
Clinical Fellow
University of British Columbia Faculty of Medicine
Vancouver, British Columbia, Canada
Presenting Author(s)
Background: Delayed umbilical cord clamping (DCC) has emerged as a standard of care at all gestational ages. It is associated with improved neonatal hemodynamic stability. Although there is evidence suggesting decreased neonatal morbidities with DCC compared to early cord clamping (ECC), the long-term renal impact of this strategy in extremely low gestational age neonates (ELGANs) remains understudied.
Objective: We hypothesized that DCC would be associated with improved two-year renal outcomes in ELGANs.
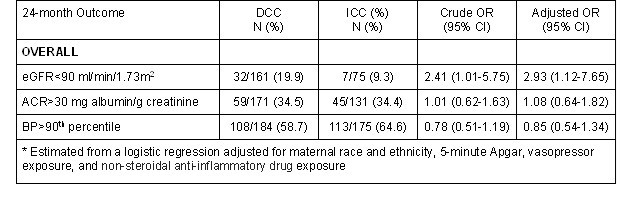
Design/Methods: We performed a secondary analysis of the Preterm Erythropoietin Neuroprotection Trial (PENUT, n=936). We included participants if umbilical cord management data were recorded, as well as estimated glomerular filtration rate (eGFR), albumin/creatinine ratio (ACR), and blood pressure (BP) data from follow-up at two years. Exposure: DCC defined as cord clamping ≥30 seconds after delivery. Primary outcomes: eGFR < 90 ml/min/1.73 m2 using the Chronic Kidney Disease in Children (CKiD) under 25 (CKiD U25) equation, ACR >30 mg albumin/g creatinine, and BP >90th percentile. We used a generalized estimating equation logistic regression model to assess the association between DCC and the two-year renal outcomes.
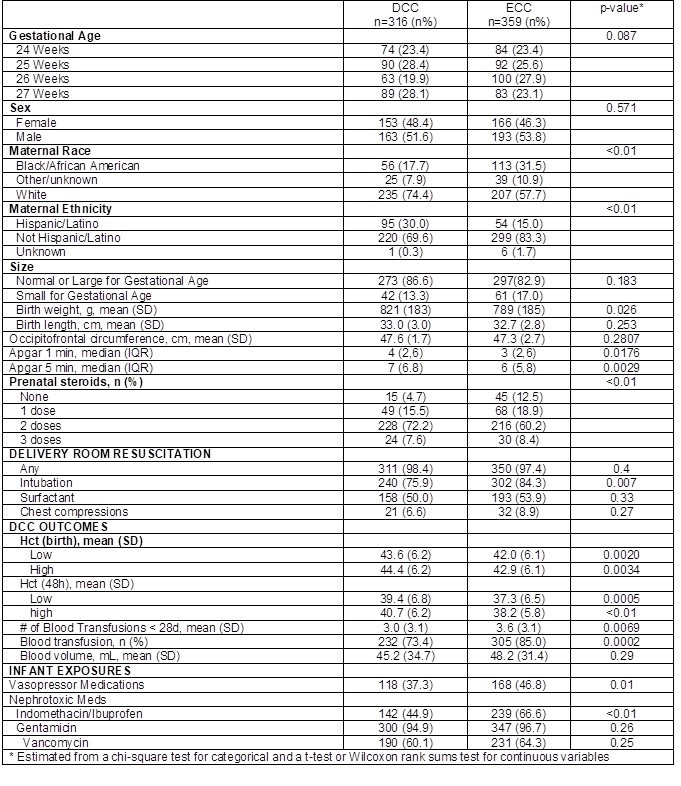
Results: Cord management data was recorded in 674 infants 24-27 6/7 weeks gestation (DCC n=316, ECC n=359), out of which 359 (53%) had 22-26 month renal outcome data recorded (DCC n=184, ECC n=175). The DCC group had higher Apgar scores at 1 and 5 minutes (p=0.02 and p< 0.01), greater exposure to prenatal steroids (p< 0.01) and higher mean birthweight (821g vs 789g, p=0.02) (Table 1). 39 (16%) infants had an eGFR < 90 at two years of age (DCC 20% vs ECC 9%) (Table 2). After adjusting for maternal race and ethnicity, Apgar scores, vasopressor exposure, and non-steroidal anti-inflammatory drug exposure, infants with DCC were nearly 3 times as likely to have decreased eGFR at 2 years compared to those with ECC (aOR 2.93, 95% [CI 1.12-7.65]); no significant associations between DCC and ACR or BP were noted (Table 2).
Conclusion(s): In contrast to our hypothesis, DCC was associated with increased rates of eGFR < 90 at 2 years compared to ECC after adjustment for significant factors. The impact of prenatal steroids and exposure to nephrotoxins on nephrogenesis and renal function in ELGANs requires further investigation. Co-morbidities like necrotizing enterocolitis, infections and need for surgical interventions may have contributed to the findings. Further research is needed to quantify the impact of cord clamping strategies on renal outcomes in this vulnerable population.