General Pediatrics: Primary Care/Prevention
General Pediatrics 4
469 - Improving Connections to Early Intervention for Urban Children with Positive Developmental Screens
Publication Number: 469.217

Caroline Kirby, MD (she/her/hers)
Developmental and Behavioral Pediatrics Fellow
Golisano Children's Hospital at The University of Rochester Medical Center
Rochester, New York, United States
Presenting Author(s)
Background:
Early intervention (EI) determines eligibility for therapeutic services to children < 3 years old who have developmental needs. In Monroe County, NY, only 50% of EI referrals result in an evaluation. Prior studies have shown that using a tracking system with follow-up from patient navigators results in more completed evaluations by EI. Our study uses a similar tracking system but with follow-up from office staff.
Objective:
For children aged 17-21 months with positive Ages and Stages Questionnaires (ASQs) at 18-month well child checks (WCC), we aimed to implement a tracking system, including a follow-up process from clinic staff to referred families. The goal of this QI project was to increase evaluations completed by EI within 2 months of referral by 20% over 14 months.
Design/Methods:
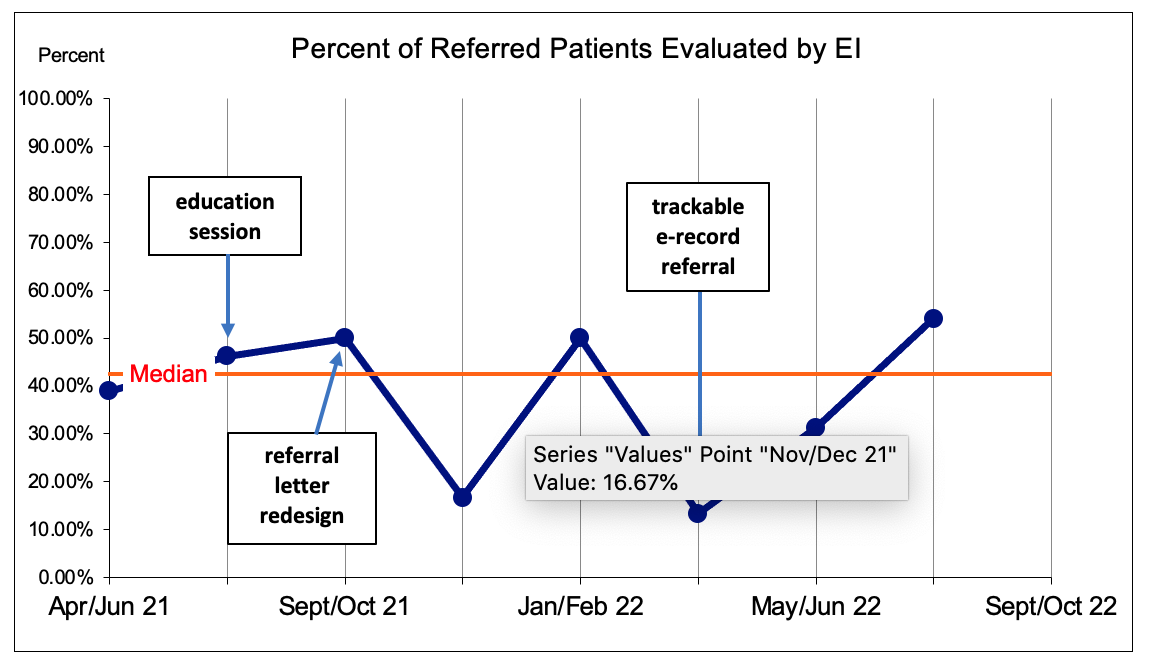
This quality improvement study was done in an urban, pediatric clinic serving 70% Black patients and 80% Medicaid insured. A key driver diagram was utilized. Our team met monthly. PDSA cycles included 1) a yearly teaching session for all clinic providers, 2) simplifying and enhancing the referral letter template to include information requested by EI, and 3) an e-record referral to track patients. Run charts were used to assess process measures, including percent of positive ASQs referred to EI and accurate descriptions of development concerns in the referral letter. The outcome measure was the percent of referred patients evaluated by EI, confirmed by receipt of an evaluation report from EI.
Results:
A total of 660 charts were reviewed over a 4-month baseline and 14-month intervention period. 88% of 18-month WCCs (580/660) had a completed ASQ. Of those, 177 (31%) screened positive. A median of 75% of patients (136/177) were referred to EI for an evaluation. There was no special cause variation for referring patients to EI (Fig 1). However, after EI education (Aug. 2021) and revision of the referral letter (Oct. 2021), a positive shift was observed in accuracy of provider descriptions in the referral letter (median 80% to 100%, Fig 2), demonstrating special cause variation. The percent of evaluations completed by EI was unchanged (median of 43% (Fig. 3)).
Conclusion(s):
A combination of education, referral template changes, and tracking system improved the quality of referrals to EI, but did not improve completed evaluations by EI. Possible reasons for low evaluation rates may reflect a period of high staff turnover (both in the clinic and at EI), as well as family and social stressors hindering evaluation completion. These results illustrate the need for family input in this process, especially for marginalized families..png)
.png)