Neonatal General
Neonatal General 5: COVID, Infections Diseases
692 - Impact of COVID-19 pandemic on neonatal hypoxic ischemic encephalopathy
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 692
Publication Number: 692.233
Publication Number: 692.233
Dongli Song, Santa Clara Valley Medical Center, San Jose, CA, United States; Angela Huang, Santa Clara Valley Medical Center, San Jose, CA, United States; Claudia V. Flores, Santa Clara Valley Medical Center, San Jose, CA, United States; Priya Jegatheesan, Santa Clara Valley Medical Center, San Jose, CA, United States
- DS
Dongli Song, MD, PhD (she/her/hers)
Neonatologist
Santa Clara Valley Medical Center
San Jose, California, United States
Presenting Author(s)
Background: Neonatal hypoxic-ischemic encephalopathy (HIE) is a leading cause of infant mortality and long-term neurological disabilities. Therapeutic hypothermia (TH) is an effective therapy for infants with moderate to severe HIE. Prenatal and perinatal care has been adversely affected during the COVID-19 pandemic.
Objective: This study aims to assess the impact of COVID-19 pandemic on neonatal HIE evaluation, treatment and outvomes.
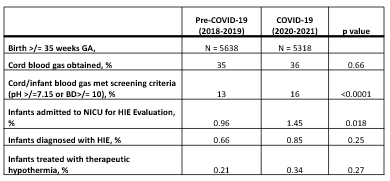
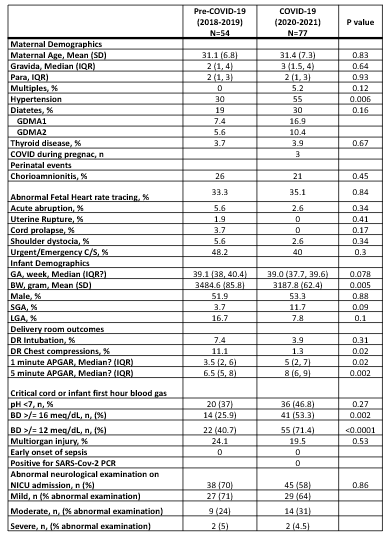
Design/Methods: This is a retrospective study comparing neonatal HIE evaluation and TH between the pre-COVID-19 (January 1, 2018, to December 31, 2019) and the COVID-19 (January 1, 2020, to December 31, 2021) periods. We used standardized HIE evaluation and TH protocols that were established in 2008. Newborns at risk for HIE were identified and evaluated based on prenatal events, cord or infant first blood gas, and newborn neurological examination. Infants with abnormal neurological examination or significant metabolic acidosis (BD >12 mmol/L) were admitted to NICU for further evaluation of HIE and eligibility for TH. Maternal and neonatal characteristics, delivery room and NICU outcomes between the two periods using chi-square, t-test, Wilcoxon (Mann Whitney) rand-sum test. The 14-year (2008-2021) data of NICU admission for HIE evaluation is illustrated in the statistical process control chart.
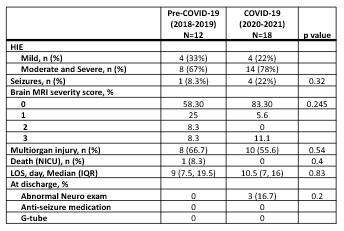
Results: From the pre-COVID period to the COVID-19 period, maternal hypertension increased from 30% to 55% (p=0.06), the proportion of the blood gases that met HIE screening criteria increased from 13% to 16% (p< 0.0001), and the proportion of infants admitted to NICU for HIE evaluation increased from 0.96% to 1.45% (p< 0.018), respectively. There was no difference in the percentages of infants diagnosed with HIE (0.66% vs. 0.85%, p=0.25) or treated with TH (0.21% vs 0.34%, p=0.27) between the two periods. There were no differences in the outcomes of the infants who received TH between the two periods.
Conclusion(s): During the pandemic period, we observed significant increases in maternal hypertension and NICU admissions for HIE evaluation, resulting in increases in mother-infant separation, medical staff workload, and medical costs. While we did not show significant increases in neonatal HIE and TH, larger studies are needed for a comprehensive assessment of the impact of the COVID-19 pandemic on neonatal HIE.