Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 5: Epi/HSR Covid-19/Potpourri
804 - Intimate Partner Violence, Depression, and Anxiety in Mothers with Infants in the Neonatal Intensive Care Unit (NICU)
Publication Number: 804.249

Sujata Desai, PhD (she/her/hers)
Research Psychologist
Pediatrix Medical Group @ Baylor Scott & White Health
Dallas, Texas, United States
Presenting Author(s)
Background:
Intimate partner violence (IPV), depression, and anxiety may significantly impact neonatal outcomes. However, the incidence of and relationships among these factors are relatively unknown in neonatal intensive care unit (NICU) mothers. The World Health Organization estimates 4-12% of women are victims of IPV during pregnancy. Other studies estimate that IPV incidence during pregnancy can range from 1-20%, but there is little IPV research with NICU mothers. Depression rates vary from 7.4% in the first trimester to 12% in the third trimester, and can also be common in NICU mothers. Postpartum depression (PPD) in NICU moms can range from 28-70%.
Objective: To determine incidence of IPV and depression/anxiety scores as well as the relationships among these variables in mothers at a community NICU.
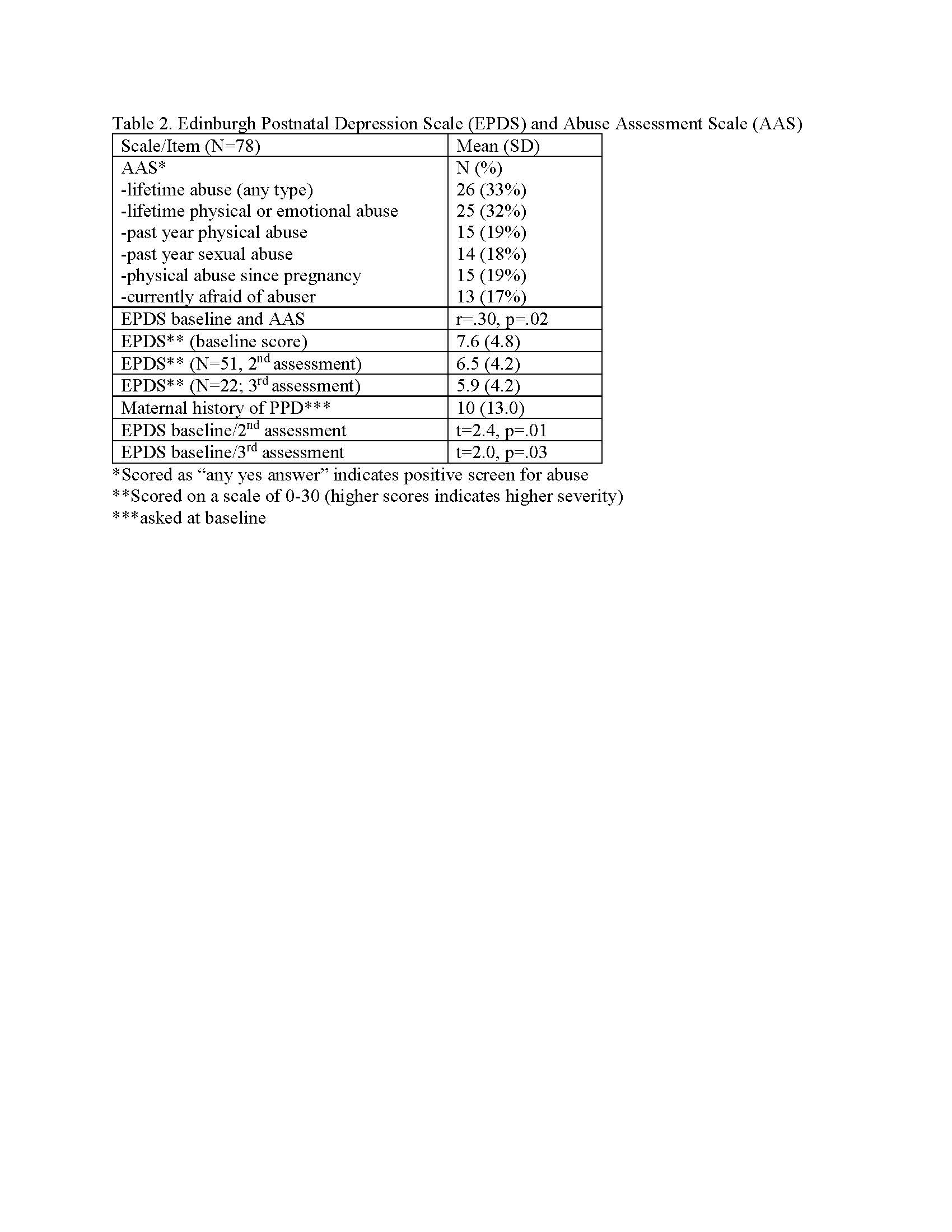
Design/Methods: In this descriptive study, each mother was consented and screened alone in a private room. Participants were given the Edinburg Postnatal Depression Scale (EPDS) and the Abuse Assessment Screening Tool (AAS) within 2 days of the neonate’s admission to the NICU. They took the EPDS a second time about two weeks later if the neonate remained in the NICU, or earlier if discharged prior to two weeks. If a neonate remained in the NICU longer, the mother was given the same survey a third time at discharge.
Results: Of 78 enrolled mothers (Table 1), 19% (15) reported abuse during pregnancy when screened with the AAS, (Table 2). In contrast, no participants reported abuse at the time of their labor and delivery admission. All mothers reporting past year abuse expressed fear of their current partner. A significant and moderate correlation emerged between abuse and baseline depression and between depression/anxiety and past year partner violence. Significant decreases with moderate effect sizes were found between the first and second EPDS and between the first and third. Multiple regression did not identify perinatal factors predictive of abuse or depression. No findings between depression and abuse emerged when comparing mothers of preterm infants (< 34 weeks) to nonpreterm (>34 weeks).
Conclusion(s): This study addresses gaps assessing IPV in NICU mothers and showed a marked difference between what participants reported in their health history at admission versus what they reported when given evidence-based surveys in a safe, private setting. These results challenge the assumption that accurate screening happens at admission using one or two yes/no questions. It is imperative that screening occurs in a safe area with evidence-based scales to improve maternal and neonatal outcomes..jpg)