Nephrology: Dialysis
Nephrology 1: AKI
259 - Correlation Between Stroke Volume Variability, Thoracic Fluid Content, and Net Fluid Balance in Pediatric Continuous Renal Replacement Therapy
Publication Number: 259.25

Anna M. Lang, BSA (she/her/hers)
Medical Student
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background:
Continuous renal replacement therapy (CRRT) is the primary dialysis modality for physiologically unstable patients. Fluid removal on CRRT should be controlled without leading to hypotension to avoid propagation of organ dysfunction related to dialy-trauma. Decreased intravascular fluid volume leads to a compensatory increase in stroke volume variability (SVV), which is predictive of hypotension in the adult population, and electro-cardiometry based measurement of thoracic fluid content (TFC) can allow for a more precise and accurate measurement of fluid balance (FB).
Objective: The objective of this study is to describe the relationships between SVV, TFC, and FB in pediatric patients receiving CRRT.
Design/Methods: Prospective single center study of pediatric CRRT patients (< 18 yr) between November 2019 and March 2021. All hemodynamic parameters as well as TFC were measured using electro-cardiometry (ICON, Osypka Medical Berlin, Germany). SVV was a percent change in stroke volume every minute averaged over the hour.
Results:
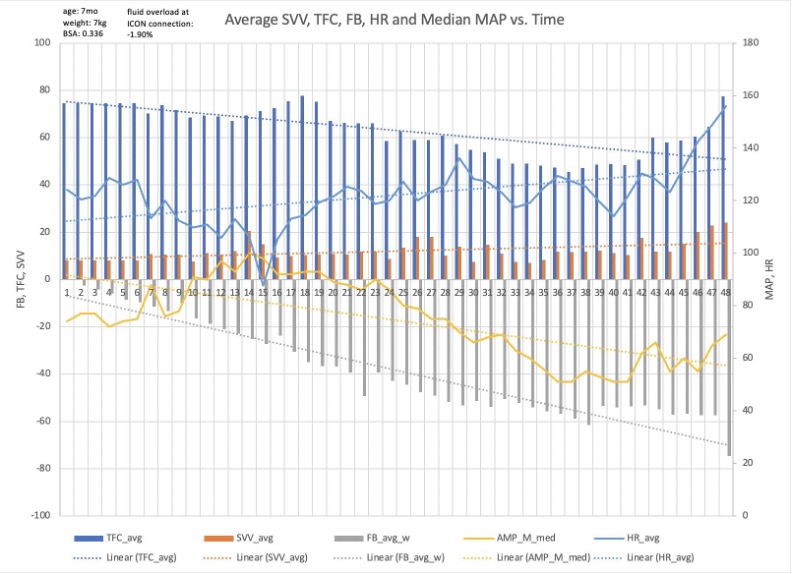
17 patients with a median age 43 months (IQR 13-122) were enrolled. The median time between CRRT start and electro-cardiometry connection was 24.5 hours (IQR 21.5-41 hours). The most common CRRT indication was acute kidney injury with fluid overload. Median fluid overload at CRRT start was 171.5 mL/kg (IQR 31.1-307.4 mL/kg) and median fluid overload at electro-cardiometry connection was 186.7 mL/kg (IQR -18.03-260.80 mL/kg). Median FB was -15.9 mL.kg (IQR -50.3 - -0.6 mL/kg), median TFC was 67.0 kΩ−1 (IQR 45.6-91.5 kΩ−1), and median SVV was 14.6% (IQR 10.3-19.3%). Initial FB and TFC were not correlated (r = 0.16, 95% CI –[0.35, 0.59], p = 0.55). FB and TFC were negatively correlated (r = -0.09, 95% CI [-0.16, -0.02], p = 0.01) over the first 48 hours; for every 1 kΩ−1 increase in TFC, total FB decreased by 0.08 mL/kg.
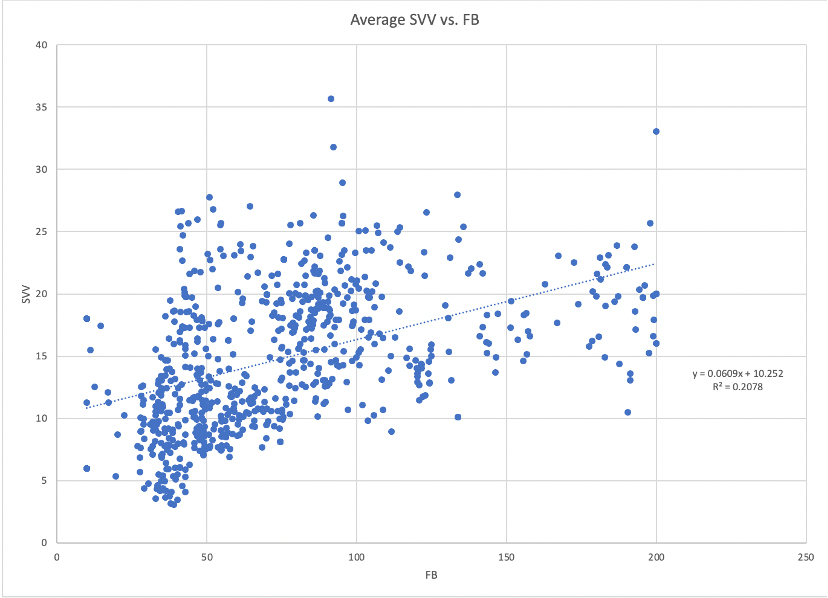
SVV and FB were negatively correlated (r = -0.30, 95% CI [-0.36, -0.23], p < 0.01). For every 1 mL/kg decrease in FB, SVV increased by 0.04%. SVV and TFC were positively correlated (r = 0.46, 95% CI [0.40, 0.51], p < 0.01). For every 1 kΩ−1 increase in TFC, SVV increased by 0.06%.
Conclusion(s):
Changes in FB were not paralleled by expected changes in TFC and SVV in pediatric CRRT. TFC might not be a reliable metric in intubated critically ill children to gauge FB. Future studies need to explore other variables that can further accurately monitor fluid balance and better anticipate possible hemodynamic crises in children on CRRT..jpg)