Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 4: Epi/HSR Utilization, Cost, Outcomes
785 - Retrospective review of survival and developmental outcomes of military infants after periviable rupture of membranes
Publication Number: 785.248

Elizabeth Okonek, MD (she/her/hers)
Neonatology Fellow
Brooke Army Medical Center
San Antonio, Texas, United States
Presenting Author(s)
Background:
Rupture of membranes (ROM) prior to viability affects 1 in 1000 births. If the fetus survives to viability, there can be significant morbidity. Previous belief was periviable ROM was incompatible with life.
Objective:
Study aims: 1) clarify survival for infants affected by periviable prolonged premature rupture of membranes (PPROM) in the military health system (MHS); 2) add to current literature on outcomes following expectant management; 3) provide data on long-term neurodevelopmental outcomes.
Design/Methods:
Retrospective matched cohort review of six level 3 military NICUs (January 2010-December 2020). Mother-infant dyads with periviable PPROM before 23 weeks gestation were included. Control infants had rupture of membranes within 24 hours of delivery and were matched 1:1 with cohort infants by birth location, gestational age, birth weight within 300 grams, and sex. Exclusion criteria include one or more major congenital anomalies, elective termination of pregnancy after periviable PPROM or expectant management but delivered prior to viability.
Results:
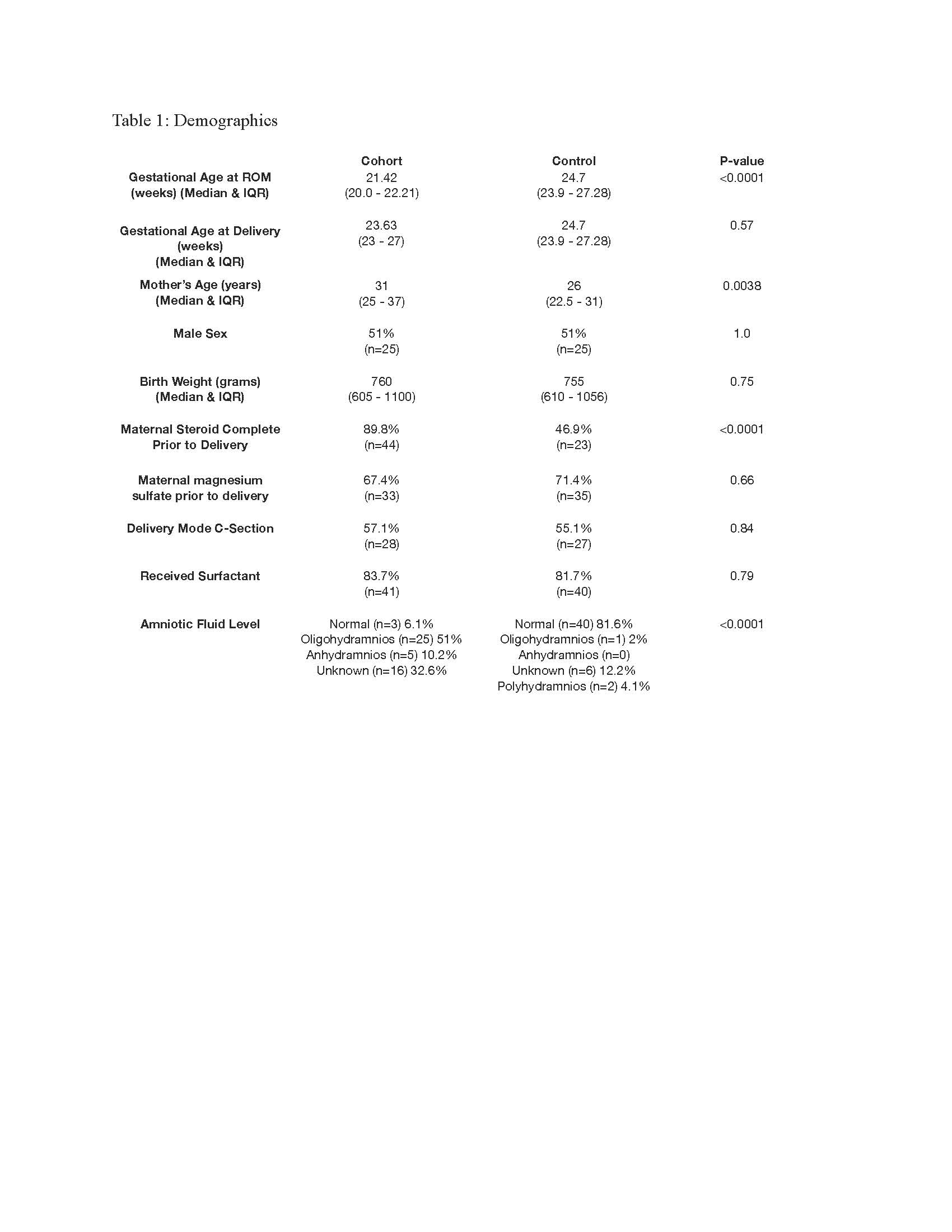
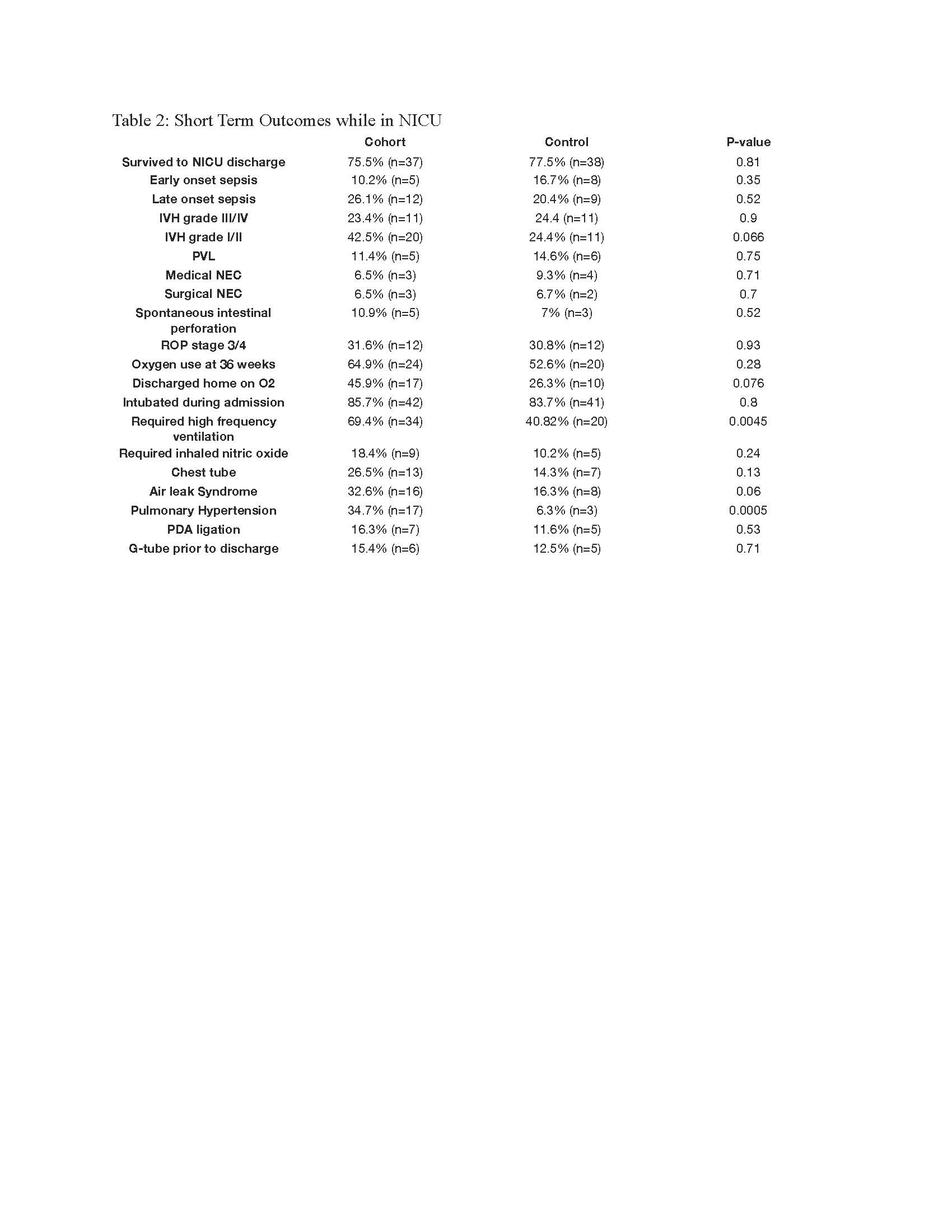
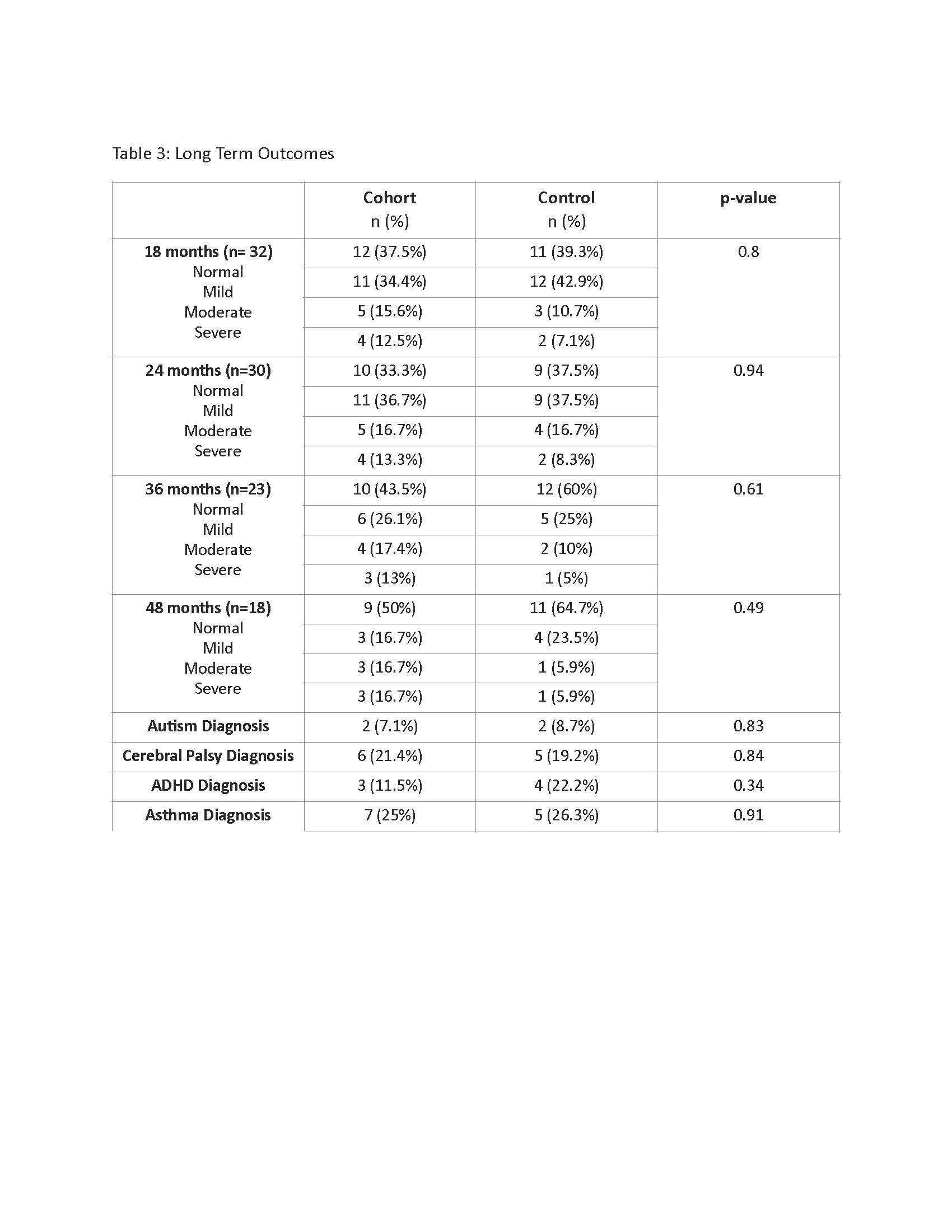
One-hundred and sixty-one cases of periviable PPROM were identified, 140 (87%) dyads opted for expectant management; 72 infants (45%) delivered after viability and 49 infants (30%) survived and met inclusion criteria. Cohort survival to NICU discharge was 75%, compared to 77% of controls (p-value 0.81). Infants that survived to NICU discharge the median ROM was 21+3 weeks gestation, delivery occurred at 24+4 weeks and birth weight of 760 grams. Cohort mother’s were older (31 vs 26 years, p-value=0.0038) and more likely to have completed course of prenatal steroids (89% vs 47%, p-value < .0001). Statistically significant short term outcomes: amniotic fluid index at delivery (p-value < .0001), pulmonary hypertension (0.0005) and high frequency ventilation (p-value 0.0045) in cohort infants, table 2. No differences regarding rates of early sepsis, grade III/IV intraventricular hemorrhage, surgical necrotizing enterocolitis, oxygen at 36 weeks or discharge home on oxygen. No statistical difference in long term outcomes at 18, 24, 36 or 48 months of age or incidence of autism, cerebral palsy, ADHD or asthma.
Conclusion(s):
Cohort survival to NICU discharge in the MHS was 75%, higher than previously reported and not statistically different from matched controls. Infants born after periviable PPROM should be delivered at centers with access to high frequency ventilation and ability to manage early pulmonary hypertension. There was no statistically significant difference in long term neurodevelopment between the groups.