Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 3: Epi/HSR Antenatal Exposures and Neonatal Outcomes
755 - Relationship between Perceived Stigma in Healthcare Settings and Psychological Distress among Individuals Who Took Opioids During Pregnancy
Publication Number: 755.246

Carla Bann, PhD (she/her/hers)
Senior Fellow of Statistics and Psychometrics
RTI International
Apex, North Carolina, United States
Presenting Author(s)
Background:
Stigma can have a detrimental effect on quality of life, including mental health. Individuals who take opioids during pregnancy may be particularly susceptible to stigma due to the potential impact of their opioid use on their unborn child. Poor maternal mental health can have a negative impact on child development; however, individuals who experience stigma may be less likely to seek help from medical professionals. The relationship between stigma and mental health among individuals who took opioids during pregnancy is not well described.
Objective:
To examine the relationship between perceived stigma in healthcare settings and psychological distress in the postpartum period in individuals who took opioids while pregnant
Design/Methods: Analyses included 107 birth mothers of opioid-exposed infants enrolled in the Outcomes of Babies with Opioid Exposure (OBOE) study. At 0-1 months post-partum, psychological distress and stigma were measured using select measures from the Patient-Reported Outcome Measurement Information System (PROMIS) and Prenatal Opioid use Perceived Stigma scale (POPS), respectively. Food insecurity, housing instability, and Adverse Childhood Experiences (ACEs) were also assessed. Linear and generalized linear mixed effect models were conducted to compare PROMIS scale scores and needs and resources by stigma, adjusting for site/location, age, race/ethnicity, marital status, education, public insurance, and parity.
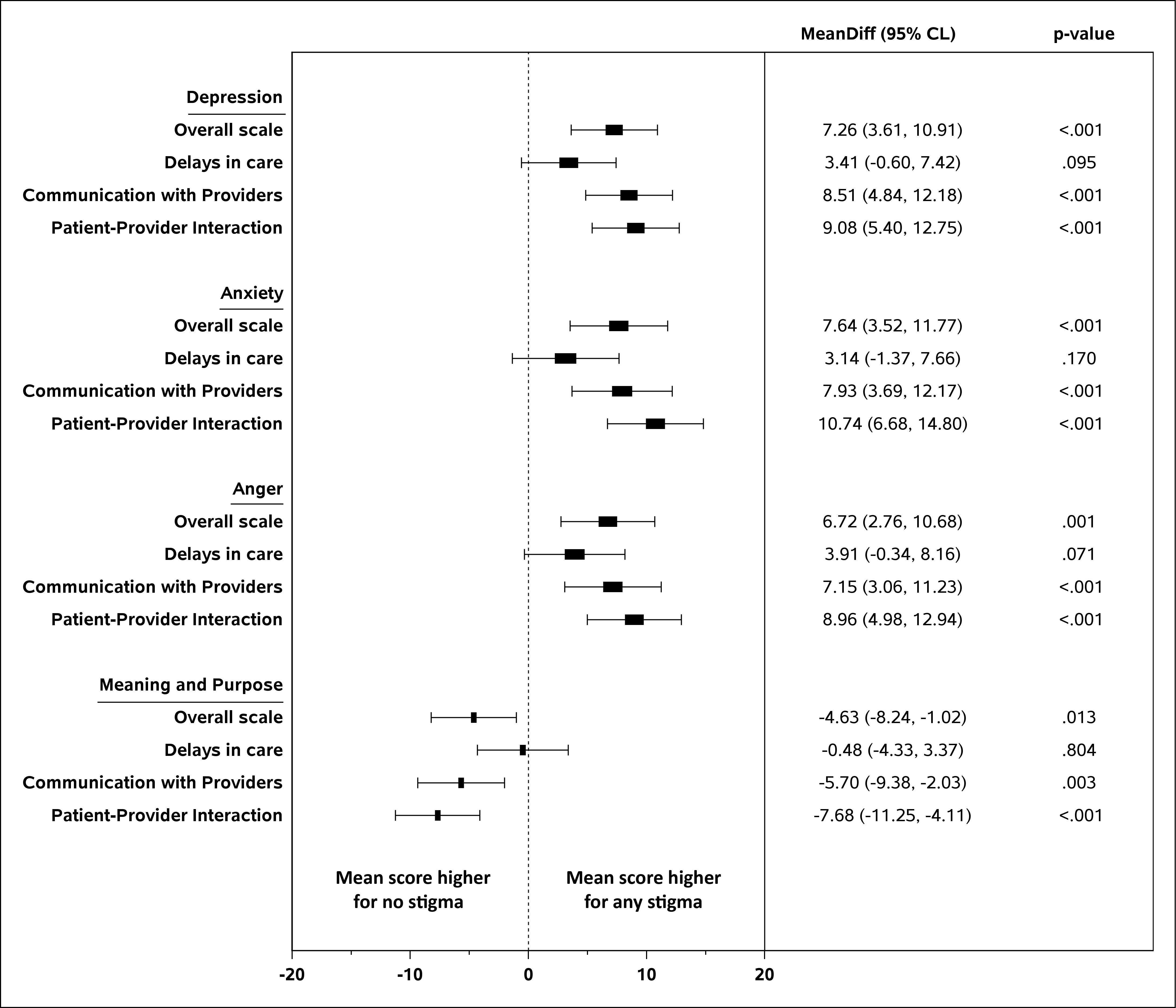
Results: Individuals reporting any stigma on the overall POPS scale had higher depression, anxiety, and anger scores, indicating greater psychological distress, in the postpartum period as compared to those reporting no perceived stigma in both the unadjusted and adjusted analyses (Table 1 and Figure 1). Furthermore, those experiencing stigma had lower meaning and purpose scores, indicating reductions in positive aspects of well-being as well. These relationships were strongest for POPS items related to communication with providers and patient-provider interactions (Figure 1). A larger proportion of those reporting any stigma as compared to no stigma screened positive for food insecurity, reported three or more ACEs, verbal or physical abuse during pregnancy, and low emotional support (Figure 2).
Conclusion(s): We observed an association between perceived stigma in the prenatal period and psychological distress in the post-partum period, suggesting a need for stigma reduction interventions and education for health care providers on trauma-informed care which could potentially impact maternal mental health in the postpartum period. .jpg)
.jpg)
