Immunizations/Delivery
Immunizations/Delivery 1
607 - Influenza, SARS-CoV-2, and routine childhood vaccines – trends in vaccine hesitancy in hospitalized children before and during the COVID-19 pandemic
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 607
Publication Number: 607.224
Publication Number: 607.224
Marisa Orbea, Texas Children's Hospital, Houston, TX, United States; Michelle Lopez, Baylor College of Medicine, Houston, TX, United States; Rachel Cunningham, Texas Children's Hospital, Katy, TX, United States; Julie A. Boom, Baylor College of Medicine, Houston, TX, United States; C. Mary Healy, Baylor College of Medicine, Houston, TX, United States; Claire Bocchini, Baylor College of Medicine, Houston, TX, United States
- MO
Marisa Orbea, MD (she/her/hers)
Fellow
Texas Children's Hospital
Houston, Texas, United States
Presenting Author(s)
Background: Vaccine hesitancy (VH) is adversely affecting the public health response to the COVID-19 pandemic. Similarly, influenza vaccine uptake is suboptimal.
Objective: We aimed to monitor trends in VH with respect to influenza, COVID-19, and routine childhood vaccines.
Design/Methods: A repeated cross-sectional survey in English and Spanish of caregiver influenza and COVID-19 knowledge, attitudes, behaviors, and associated VH among hospitalized children 6 mo-18 yrs at a large pediatric hospital. We enrolled over 4 influenza seasons (S); 2019-2020(S1), 2020-2021(S2), 2021-2022(S3), 2022-2023(S4). In S4, we targeted caregivers of children 6 mo-11 yrs. VH was assessed using the Parent Attitudes about Childhood Vaccines (PACV) survey; PACV score ≥ 50 denoted VH.
In S4, a messaging intervention was piloted. Caregivers watched a COVID-19 educational video; half watched a second video featuring a family adversely impacted by COVID-19. Caregivers completed a survey to assess acceptance and efficacy of the video(s) in increasing intent to vaccinate their child.
Results: Across seasons, ≥ 92% of caregivers approached were enrolled. Most caregivers (47%) identified as Hispanic/Latino, 34% as White, and 19% as Black. By report, 94% of children in S1, 91% in S2, 91% in S3, and 88% in S4 were up-to-date with routine childhood vaccines. Based on PACV survey score, 13% were VH in S1, 17% in S2, 19% in S3, and 22% in S4 (p=0.08).
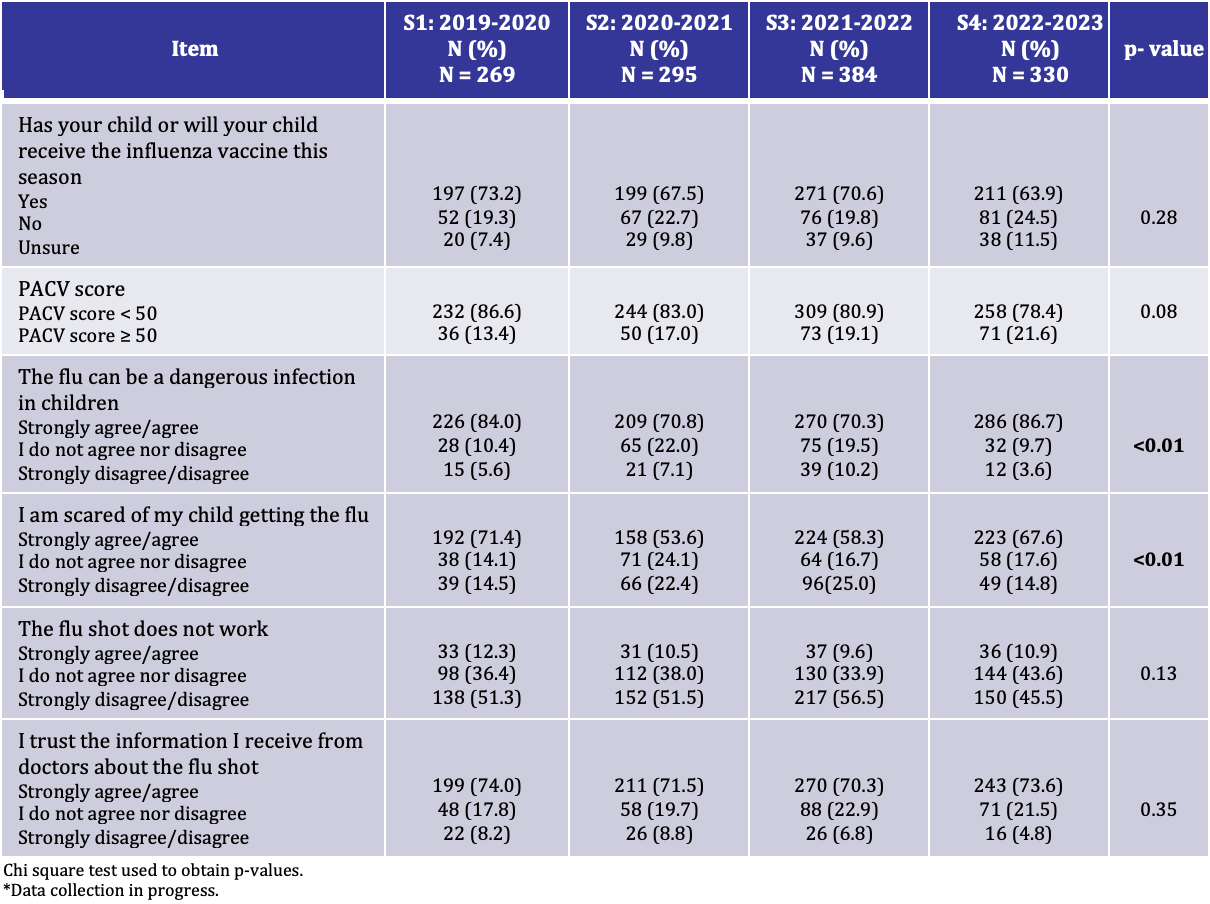
Almost 69% of caregivers planned to/gave their child influenza vaccine across seasons. During S2-3, fewer caregivers believed “flu can be a dangerous infection in children,” and reported, “I am scared of my child getting the flu” (p< 0.01). Decreased concern recovered in S4 but did not translate to increased vaccine uptake (Table 1).
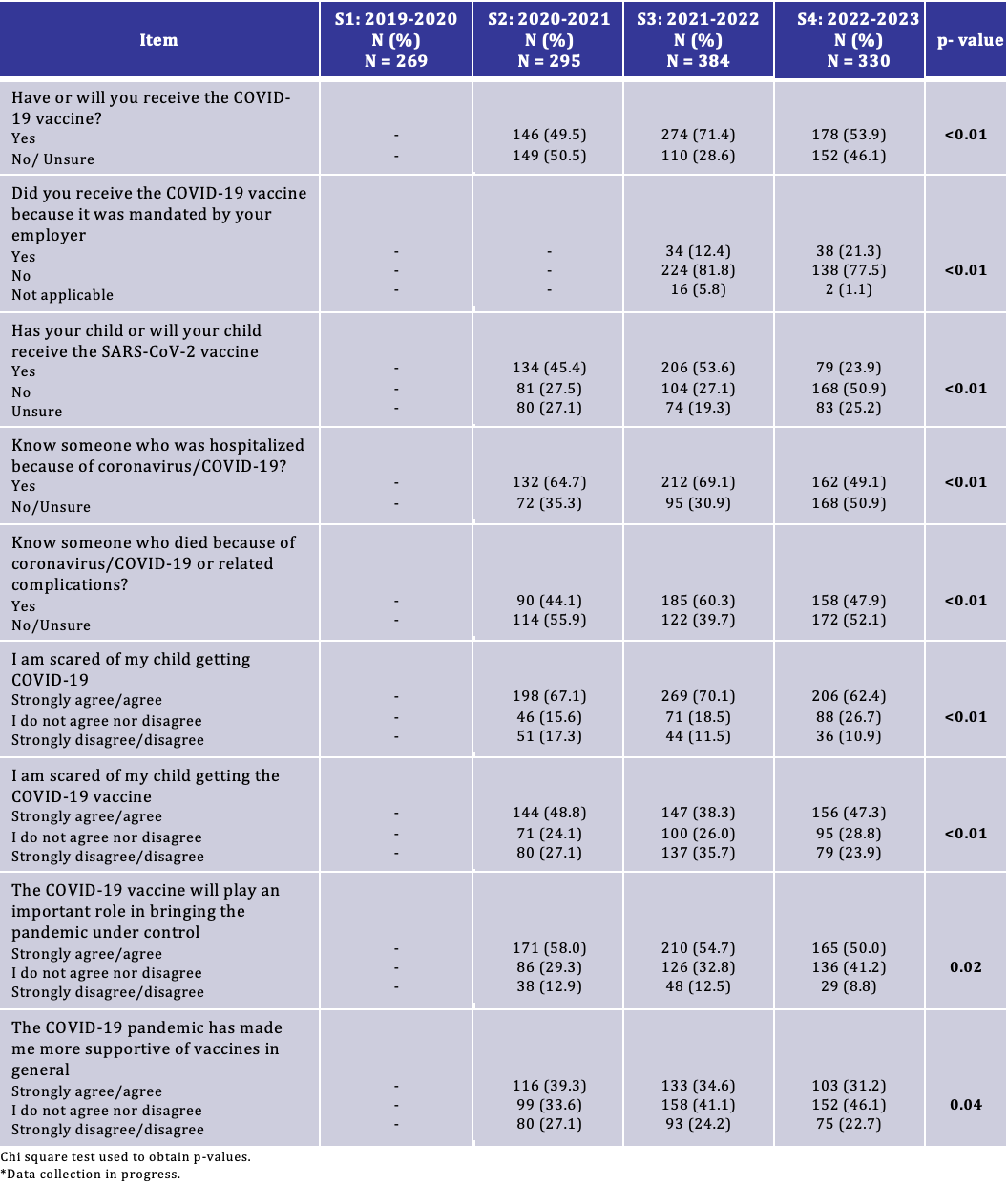
Caregivers were less scared of their child getting COVID-19 and more scared of them getting the vaccine in S4. Fewer caregivers in S4 were willing to receive the COVID-19 vaccine; 46% in S2, 54% in S3, and 24% in S4 had/planned to vaccinate their child (Table 2).
Of 328 caregivers, 241 (73.5%) liked the educational videos and 51.8% thought they were helpful when considering the COVID-19 vaccine for their child. Similarly, 72.4% liked the family story and 51.5% thought it was helpful.
Conclusion(s): Our results suggest that VH may be increasing. During S2-3, caregivers were less concerned about influenza. Concern regarding influenza is back to pre-pandemic levels (S4), but vaccine acceptance has not recovered. Vaccine uptake against COVID-19 remains suboptimal. Educational videos may help caregivers when deciding about the COVID-19 vaccine for their child.