Breastfeeding/Human Milk
Breastfeeding/Human Milk 3: Human Milk Bioactives and Composition
24 - Lactoferrin as a potential neuroprotective strategy for the developing preterm brain
Publication Number: 24.201
.jpg)
Agata Atayde, MPH (she/her/hers)
Graduate Student
Brigham and Women’s Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Lactoferrin (Lf) is an immuno-modulatory nutrient in human milk that may protect the developing preterm brain from injury, promote recovery, and/or enhance development during the neonatal intensive care unit (NICU) hospitalization.
Objective:
To determine the associations of human milk lactoferrin exposure during the first postnatal month with brain structure and injury, as measured by structural magnetic resonance imaging (MRI) at term equivalent age.
Design/Methods:
In a single-center cohort of 43 infants born < 32 weeks’ gestation, we collected human milk samples at 14 and 28 days of chronologic age and measured Lf by electrochemiluminescence multiplex immunoassay using the mesoscale discovery platform Lf U-plex assay. We averaged 14- and 28-day Lf concentrations to create a summary measure of Lf exposure. We obtained 3T quantitative brain MRI scans at term-equivalent age and analyzed them for total and regional brain volumes and global brain abnormality scores (Kidokoro, 2013). We used median regression to compare outcomes between infants exposed to low (bottom tertile, range 0.06 to 0.13 mg/ml) vs. high (top tertile, range 0.22 to 0.38 mg/ml) Lf, adjusting for gestational age (GA), birth weight z-score, sex, and postmenstrual age at MRI scan (Table 2). We adjusted for mean protein intake (g/kg/day) in a separate model to investigate its potential confounding.
Results:
Mean gestational age at delivery was 27.9 ± 2.3 weeks and 48.8% of infants were male (Table 1). The concentration of human milk Lf ranged from 0.06 to 0.38 mg/mL, median 0.18 mg/mL (Figure 1). Compared to infants exposed to low Lf, infants exposed to high Lf had an additional 43.9 cc (95% CI: 7.6, 80.4) larger total brain volume, 48.3 cc (95% CI: 12.1, 84.6) larger cortical gray matter, and 3.8 cc (95% CI: 0.7, 7.0) larger deep gray matter volume (Model I, Table 2). Other regional brain volumes were not statistically different between groups. Further adjustment for mean protein intake slightly attenuated estimates (Model II, Table 2). Infants exposed to high vs low Lf had lower global brain abnormality scores (1.8 vs. 3.2, respectively), indicating fewer abnormalities, but results were not statistically significant (P=0.618).
Conclusion(s):
Higher human milk Lf exposure during the NICU hospitalization was associated with larger brain size. These findings support Lf’s role in protecting and/or promoting recovery from brain injury and enhancing brain development. Lf supplementation may have potential as a neuroprotective strategy for this vulnerable infant population.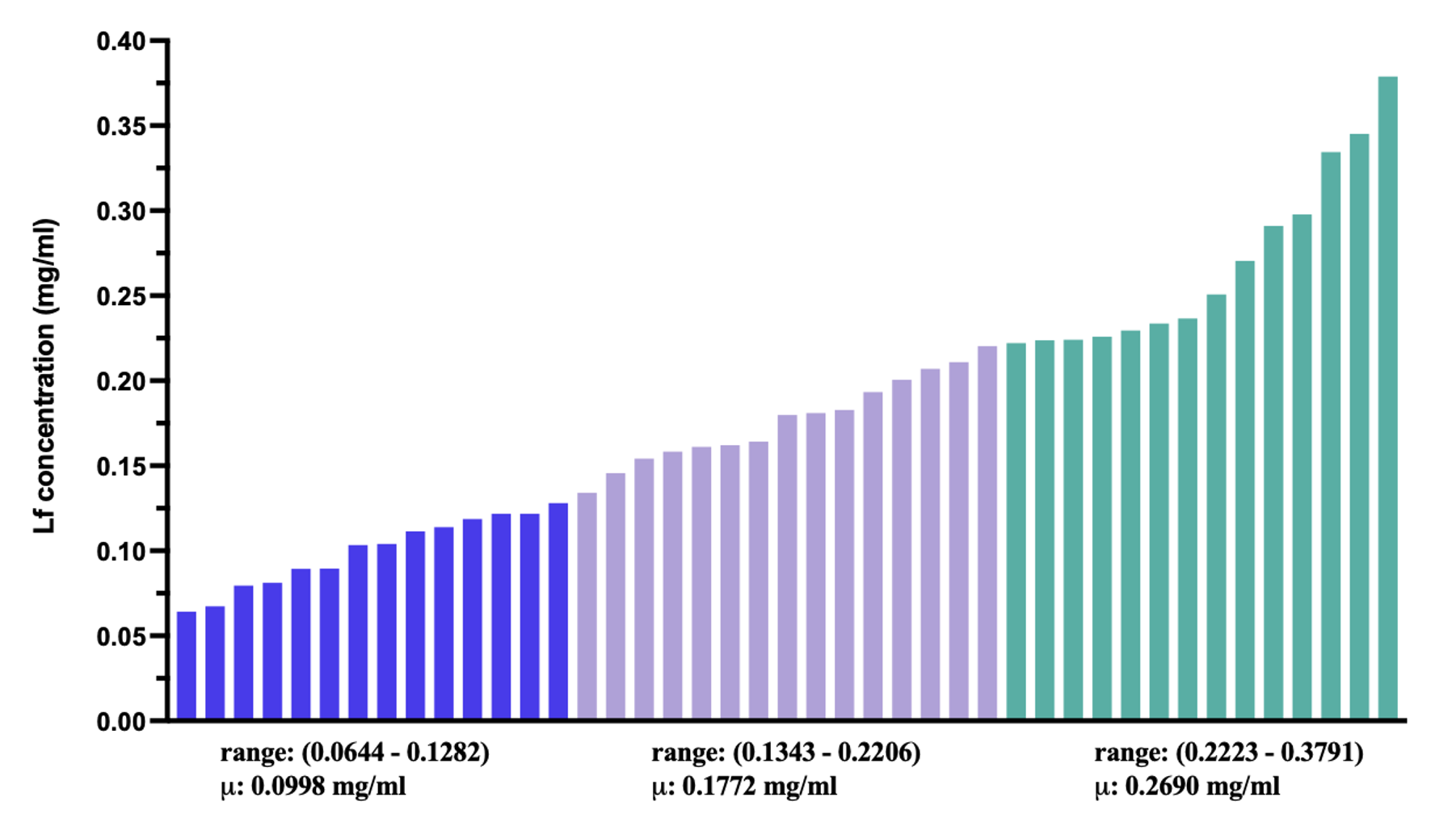
.png)
.png)
