Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 5: Predicting Necrotizing Enterocolitis, Gut Health, and Oral Feeding
100 - "NEC" is a Misnomer: Clinical Phenotypes of Acquired Neonatal Intestinal Injury Using Machine Learning
Publication Number: 100.237

Daniel R. Gipson, MD
Neonatology Fellow
University of Florida College of Medicine
Gainesville, Florida, United States
Presenting Author(s)
Background:
Many acquired neonatal intestinal pathologies are grouped under the diagnosis necrotizing enterocolitis (NEC). Over the years, other labels have been added to the differential diagnosis, including spontaneous intestinal perforation (SIP), food protein-induced enterocolitis syndrome (FPIES), dysmotility and feeding intolerance. Overlapping presentations of these different pathologies limits diagnostic accuracy, prevents progress, and limits preventative and therapeutic strategies.
Objective:
This study aims to examine classification of acquired neonatal intestinal pathologies using unsupervised machine learning.
Design/Methods:
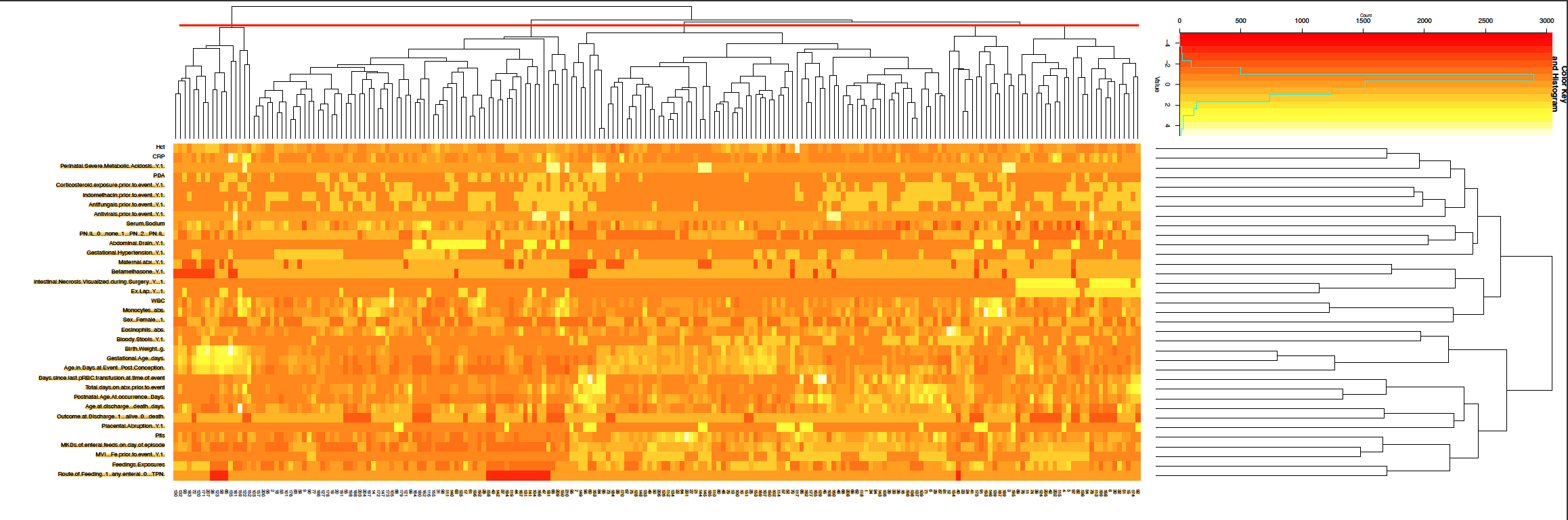
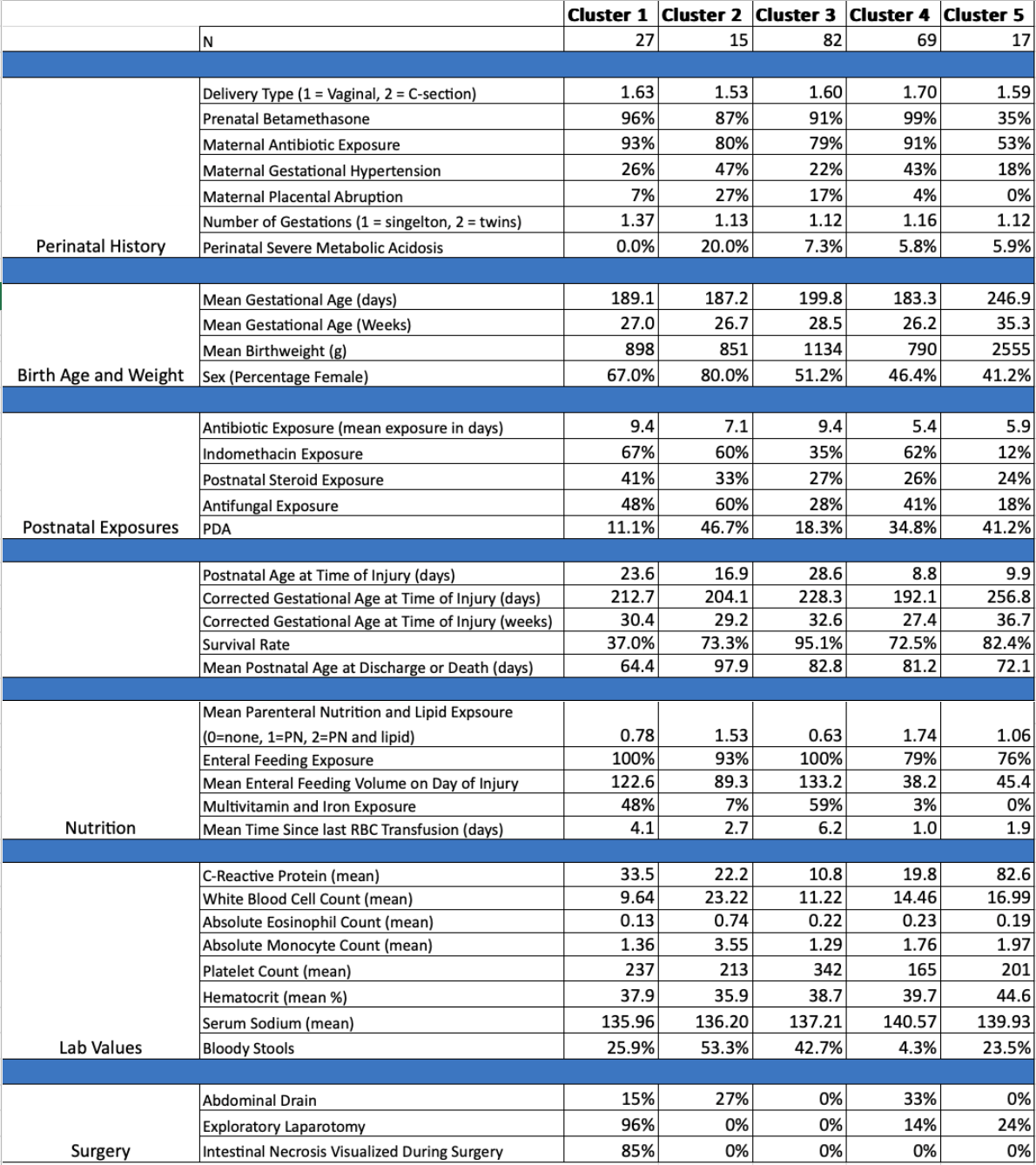
Data was collected via chart review and evaluated using unsupervised machine learning and hierarchal clustering. All columns were standardized, and a hierarchical clustering algorithm was used to identify five major clusters. The Wilcoxon rank sum test was used to identify significant features associated with each cluster.
Results:
183 infants were included in the dataset, with 27 episodes of repeat intestinal injury. Thus, 210 episodes of intestinal injuries were included in the analysis. Five clusters with unique features were identified. Cluster 1 was a “surgical necrosis” cluster (n=27 episodes) with a median gestational age (GA) of 25w6d, injury occurring at a median of 20 days of life, and a notably high mortality of 63%. Cluster 2 was a “leukocytosis” cluster (n=15 episodes) with a median GA of 25w5d, injury occurring at a median of 15 days of life, a mean leukocyte count of 23.2 x 109/L, and highest rate of bloody stools. Cluster 3 was a “non-surgical” cluster (n=82 episodes) with median GA of 28w1d, injury occurring at a median of 26 days of life, the highest enteral feeding volume exposure, highest survival rate, and lowest surgical rate at 0%. Cluster 4 was a “small with early injury” cluster (n=69 episodes) with a median GA of 25w6d, injury occurring at a median of 6 days of life, lowest mean birth weight at 789 g, lowest enteral feeding volume exposure, least antibiotic exposure, and highest rate of abdominal drain placement. Cluster 5 was a “mature with early injury” cluster (n=17 episodes) with median GA of 36w0d, injury occurring at a median of 5 days of life, notably low enteral feeding volume exposure considering GA, and highest mean CRP at 82 mg/L.
Conclusion(s): “NEC” is an inadequate label for multiple gastrointestinal pathologies encountered in neonates. We propose a revised paradigm that employs machine learning to reexamine and reclassify acquired intestinal pathologies, which is critical to strive for effective preventative and therapeutic strategies.