Nephrology: Clinical
Nephrology 1: AKI
252 - Tandem Continuous Renal Replacement Therapy and Therapeutic Plasma Exchange in Pediatric Acute Liver Failure
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 252
Publication Number: 252.25
Publication Number: 252.25
Caroline V. Jackson, Seattle Children's, Seattle, WA, United States; Kristen Carlin, Seattle Children's, Seattle, WA, United States; Niviann M. Blondet, Seattle Children's, Seattle, WA, United States; D. Ian. Jordan, Seattle Children's, Seattle, WA, United States; Larissa Yalon, Seattle Children's Hospital, Seattle, WA, United States; Jordan Symons, University of Washington School of Medicine, Seattle, WA, United States; Shina Menon, University of Washington School of Medicine, Seattle, WA, United States
.jpg)
Caroline V. Jackson, MD (she/her/hers)
Fellow
Seattle Children's
Seattle, Washington, United States
Presenting Author(s)
Background: Pediatric acute liver failure (ALF) and acute on chronic liver failure (ACLF) are associated with significant morbidity and mortality. These patients often require extracorporeal blood purification modalities as a bridge to recovery or liver transplantation. Tandem continuous renal replacement therapy (CRRT) and therapeutic plasma exchange (TPE) can provide clearance of water soluble and protein bound toxins, serving as a bridging therapy. Limited data are available on the outcomes of patients treated with tandem therapies.
Objective: To describe clinical characteristics and outcomes of patients requiring CRRT and TPE for ALF/ACLF.
Design/Methods: Retrospective cross-sectional single center study of 23 patients from 2015-2022 with ALF/ACLF who underwent CRRT and TPE.
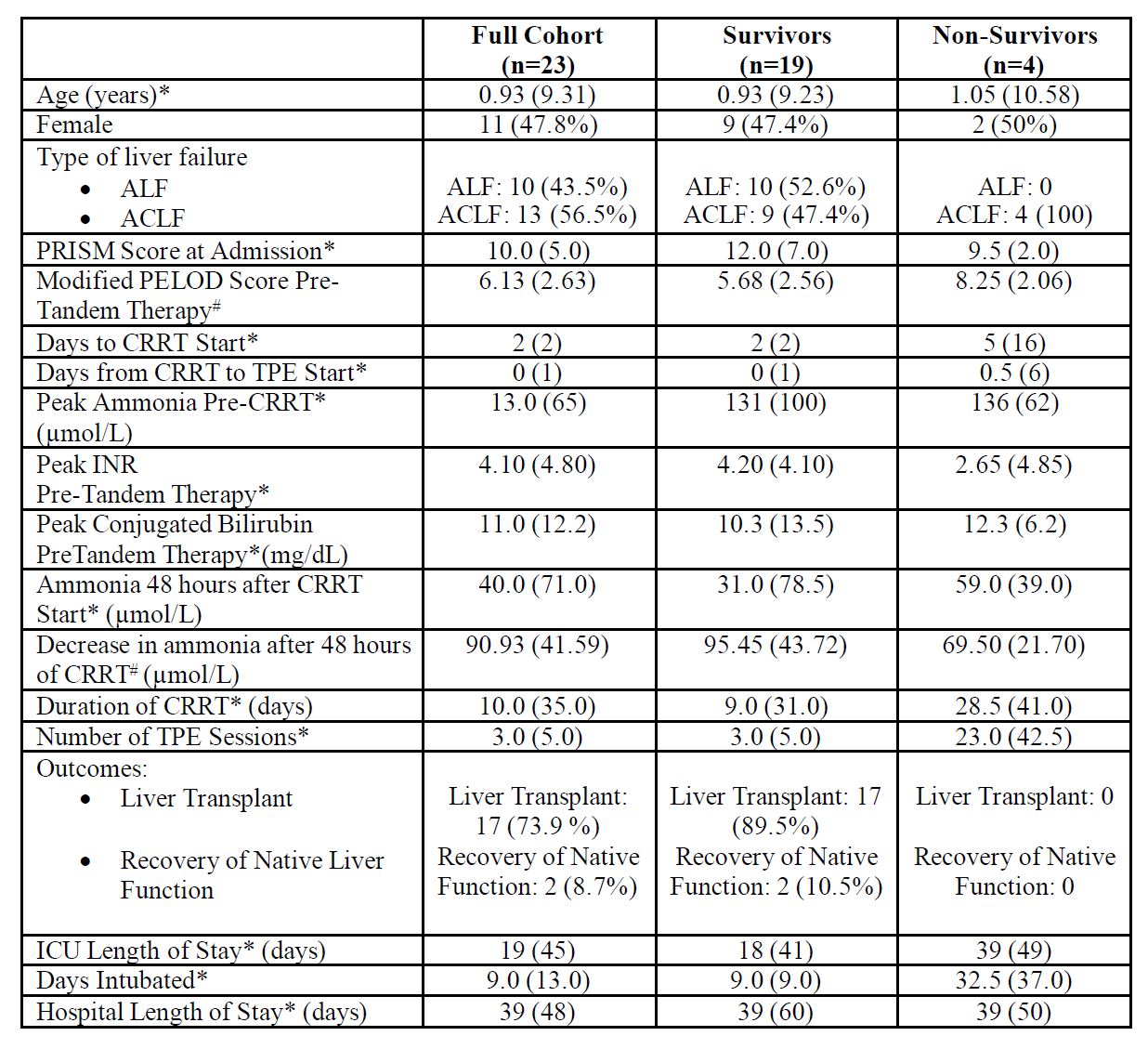
Results: The median (IQR) age was 0.93 years (9.31), range 16 days-20 years, 48% female (Table 1). Ten (43%) had ALF, and the remaining ACLF. AKI as an indication for starting CRRT was noted in 5 (22%), and hyperammonemia and/or hepatic encephalopathy in 18 (68%). Liver transplant was done in 17 (74%), 2 recovered native liver function, and 4 died while awaiting transplantation. All 4 deaths were in patients with ACLF. For the full cohort, CRRT was started at a median of 2 days from ICU admission, and TPE was started on the same day as CRRT in most. The median duration of CRRT was 9 days in survivors vs 29 days in non-survivors, and the corresponding number of TPE sessions were 3 and 23. Median peak ammonia pre-CRRT was 131 µmol/L for the whole cohort. The mean (SD) drop in ammonia after 48 hrs of CRRT was 95.45 (43.72) µmol/L in survivors and 69.50 (21.70) µmol/L in non-survivors (p 0.26). The survivors had 0 median co-morbidities compared to 2.5 in non-survivors [aOR(95%CI) for mortality risk of 2.518 (1.100- 5.766), p 0.028].
Conclusion(s): In this cohort of 23 pediatric patients with ALF or ACLF who received tandem CRRT and TPE, 83% survived with a liver transplant or recovered with their native liver function. Survival was 100% in patients with ALF, but only 70% in those with ACLF. After adjusting for age, each additional comorbidity increased the risk of mortality by 2.5 times.