Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 3: Gut Health Clinical Research
73 - Early Versus Late Feeding in Preterm neonates with Absent or Reversed End Diastolic Flow on Antenatal Umbilical Doppler study: A Randomized Controlled Trial
Publication Number: 73.235
- AA
Astha Amrit, DrNB (she/her/hers)
Student
B. J. Wadia Hospital for Children
Mumbai, Maharashtra, India
Presenting Author(s)
Background:
Enteral feeding in preterm neonates with abnormal antenatal dopplers has been a topic of debate for years. These neonates are at higher risk of developing feed intolerance and Necrotizing Enterocolitis (NEC) . There is limited evidence from randomized controlled trials regarding the appropriate timing and rate of increase of feed in such neonates.
Objective:
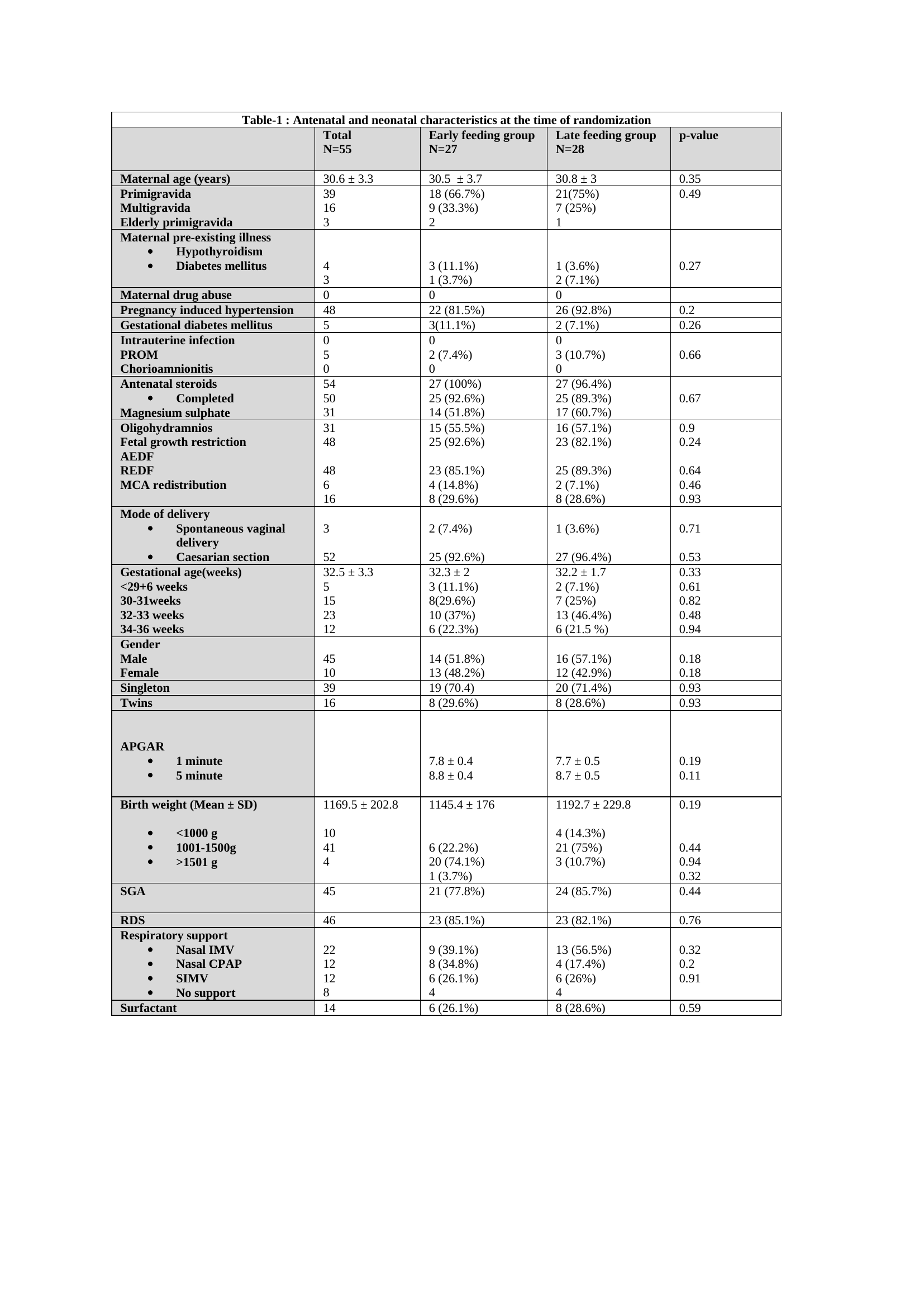
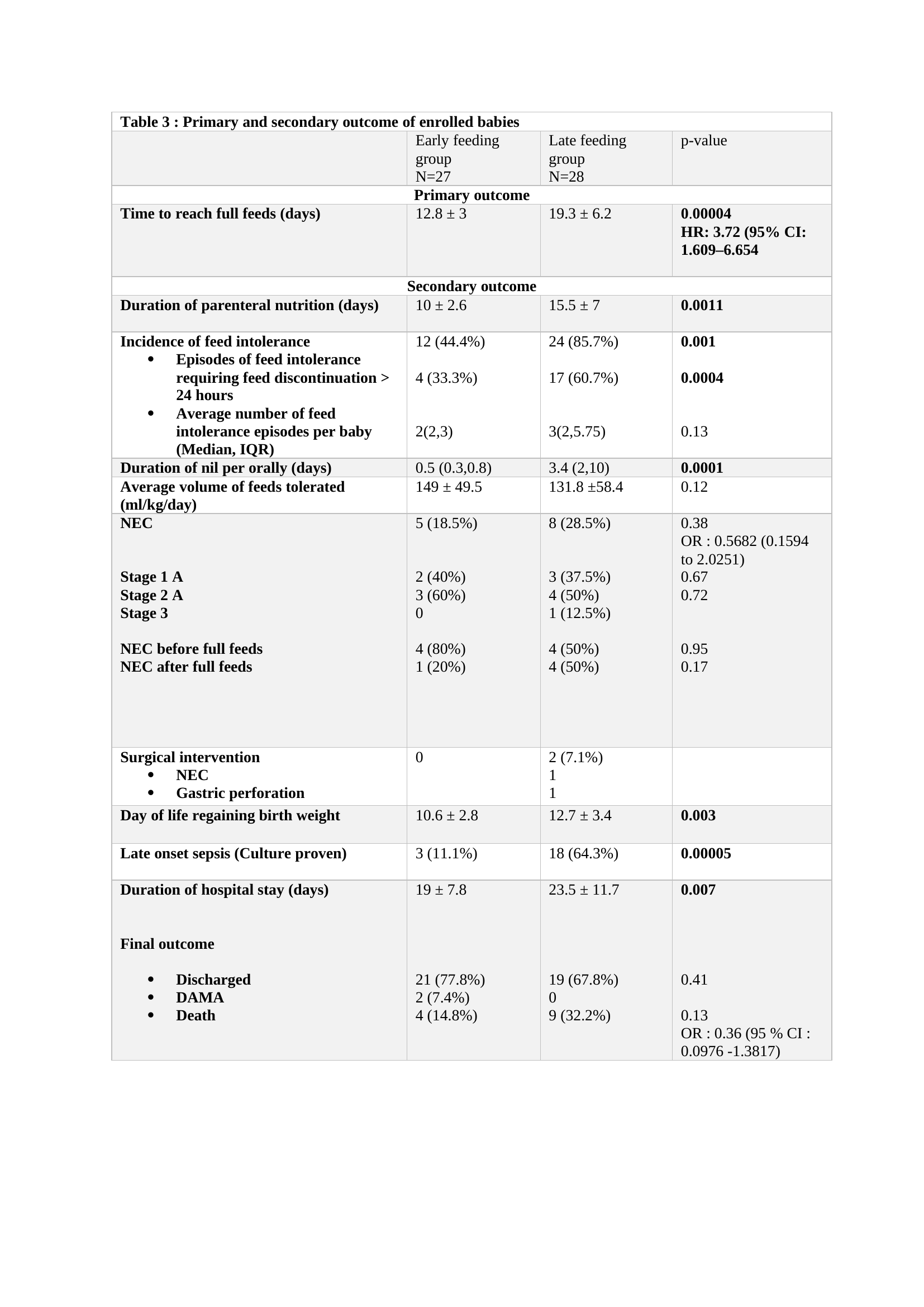
The primary objective was to study effect of early versus late feeding in preterm neonates with Absent or Reversed End Diastolic Flow (AREDF) in umbilical artery on antenatal Doppler with respect to time taken to reach full feeds. Secondary objectives included feed intolerance , NEC, time taken to regain birth weight, duration of parenteral nutrition, late onset sepsis and duration of hospitalization.
Design/Methods:
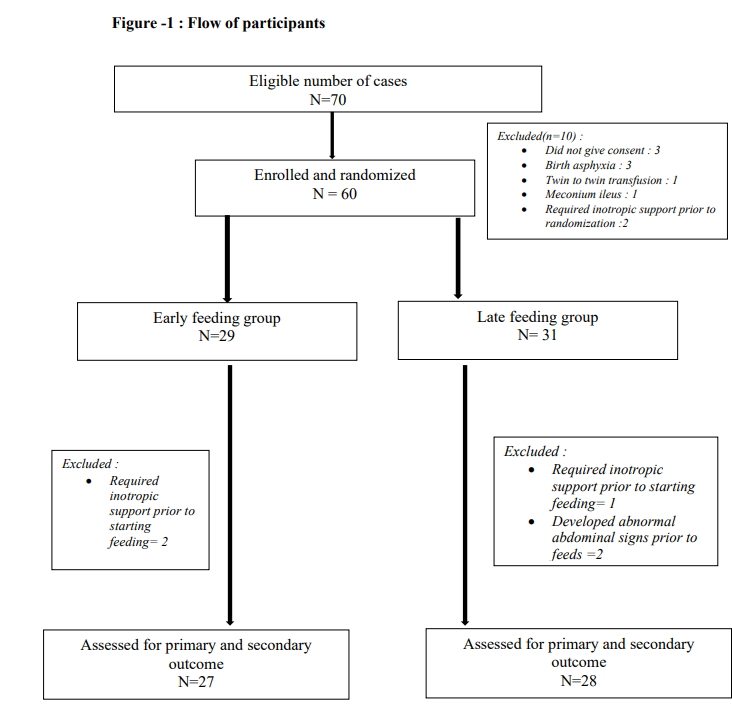
This open label randomized controlled trial was conducted in a tertiary care neonatal intensive care unit where 60 neonates were randomized to either early feeding group (n=29) and late feeding group (n=31) within 6 hours of life. Feeding was initiated as per pre-defined feeding protocol.
Results:
Average time taken to reach full feeds was 12.8 days in early and 19.3 days in late group ( mean difference: 6.5 days , Hazard ratio: 3.72 (95% Confidence Interval (CI): 1.609–6.654)); p-value: 0.001. The incidence of feed intolerance was significantly lesser in the early group (44.4%) than late group (85.7%), p-value: 0.001. The incidence of NEC was lower in the early feeding group than late feeding group (18.5% versus 28.5%, Odds ratio: 0.5682 , 95 % CI: 0.1594 to 2.0251). None of the babies in the early group had severe NEC (stage 2b and above). The average duration of parenteral nutrition was higher in late group than early group ( 15.5 days versus 10 days) and was statistically significant, p-value: 0.0011. Incidence of late-onset sepsis was also higher in late group i.e. 64.3 % versus 11.1% and was statistically significant, p-value: 0.00005. The average time to regain birth weight was 2 days earlier in the early feeding group (10.7 versus 12.9 days ) and was statistically significant (p-value: 0.003). Early feeding group babies had a lesser duration of hospital stay (19 versus 23.5 days, p-value: 0.007).
Conclusion(s):
We conclude that early feeding within 24 hours of life in preterm neonates born with AREDF is safe and allows babies to reach full enteral feeding without increasing the risk of NEC and protects from complications of prolonged parenteral nutrition