Immunizations/Delivery
Immunizations/Delivery 1
605 - Unvaccinated adolescents’ COVID-19 vaccine intentions: Implications for public health messaging
Publication Number: 605.224

Courtney Gidengil, MD, MPH (she/her/hers)
Senior Physician Policy Researcher
RAND Corporation
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Low rates of COVID-19 vaccine uptake among U.S. adolescents contribute to excess morbidity and mortality from COVID-19 infection. To date, much of the research on vaccine intentions has only assessed parents’ perspectives about their children. Understanding adolescents’ intentions and information sources on COVID-19 vaccination may help in designing effective communications to promote uptake.
Objective:
We assessed differences in intention and trusted sources of COVID-19 vaccine information between unvaccinated vaccine-acceptant and vaccine-hesitant U.S. adolescents using national survey data.
Design/Methods:
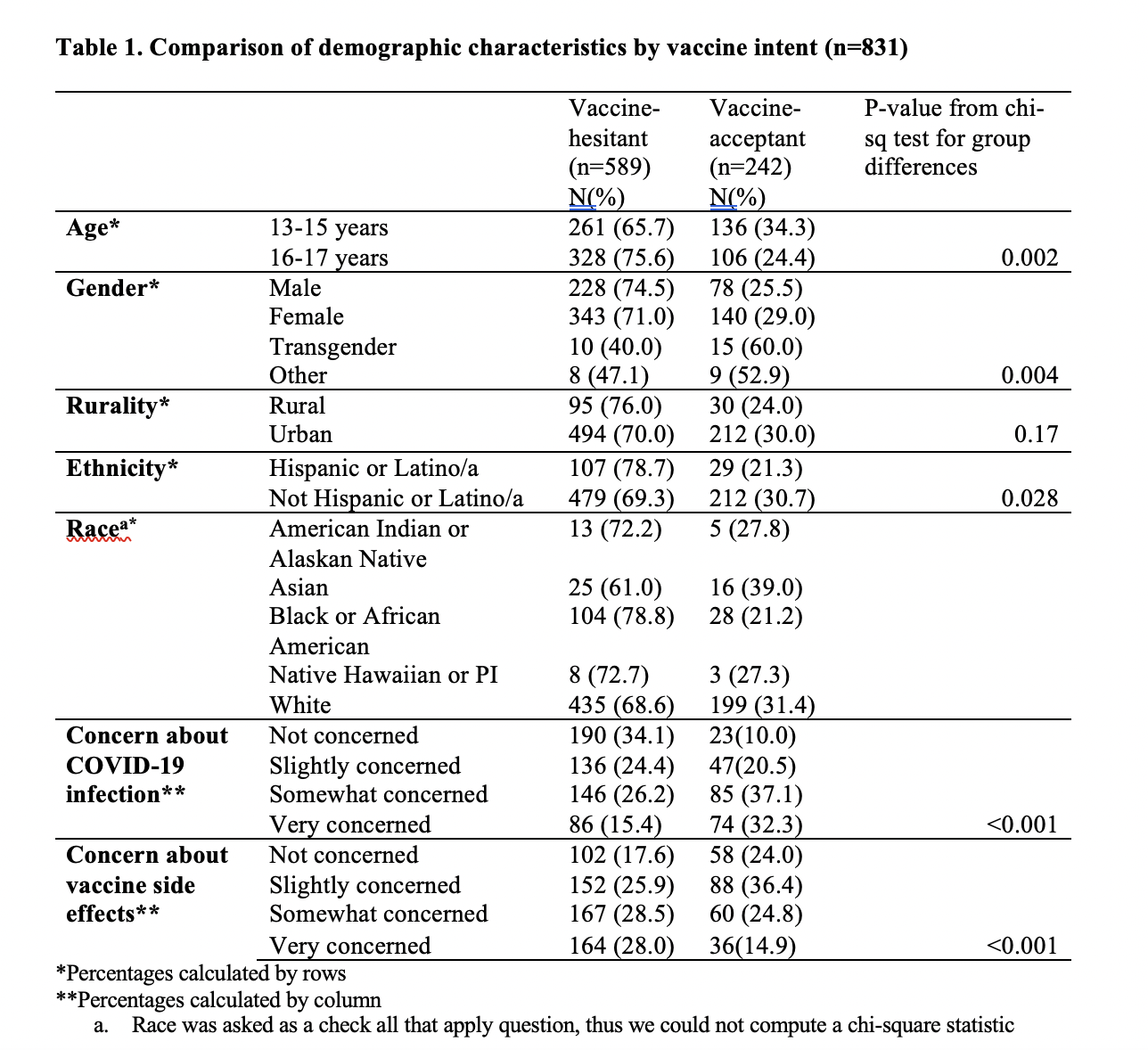
Adolescents, aged 13-17, were recruited through an online survey panel in April 2021. A total of 1,927 adolescents completed screening and our final sample included 985 responses. We only analyzed data from unvaccinated adolescents (n=831). COVID-19 vaccination intent (“vaccine-acceptant” defined as “definitely will” get a COVID-19 vaccine and any other response classified as “vaccine-hesitant”) was our primary measure. Secondary measures included reasons for intending or not intending to get vaccinated and trusted sources of information about COVID-19 vaccination. We calculated descriptive statistics and used chi-square tests to assess potential differences between vaccine-acceptant and vaccine-hesitant adolescents.
Results:
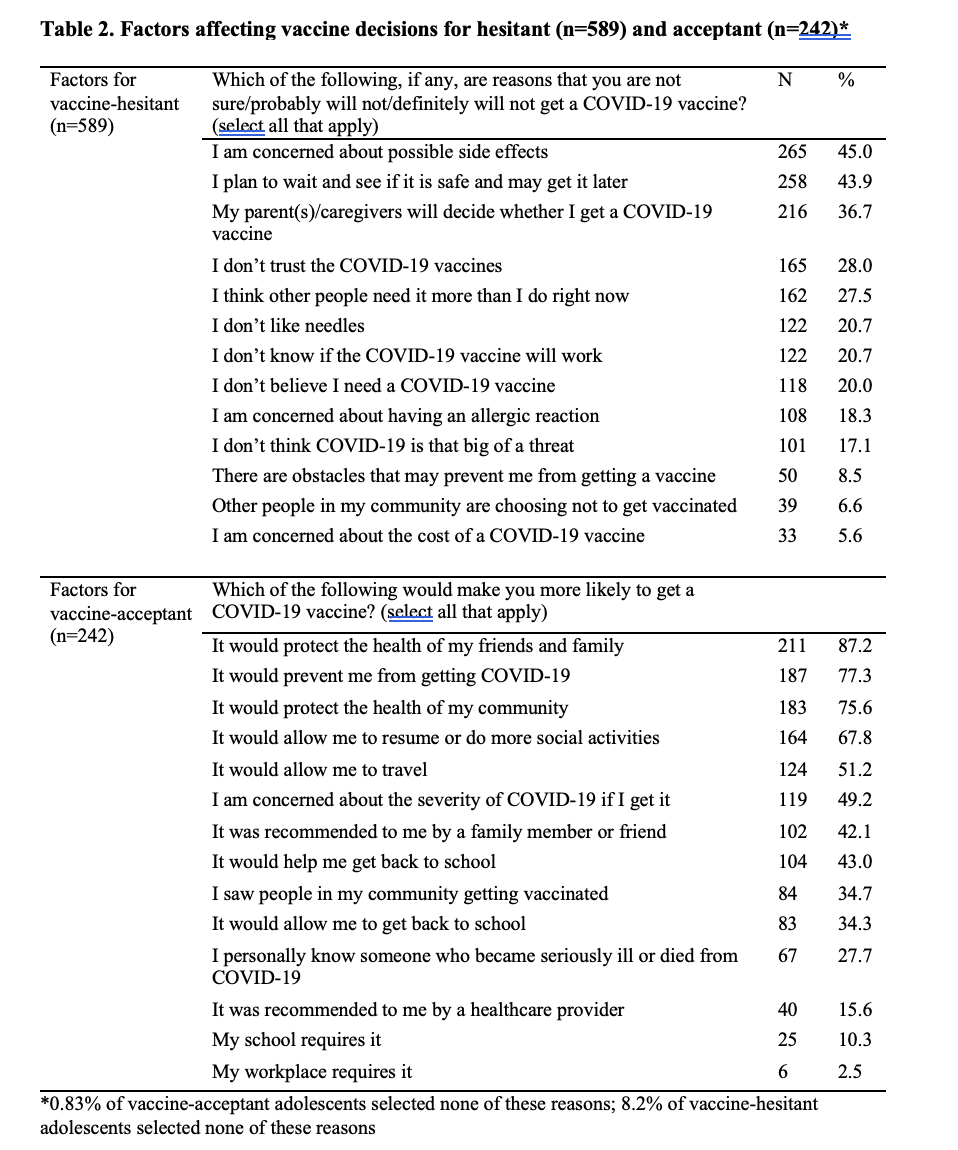
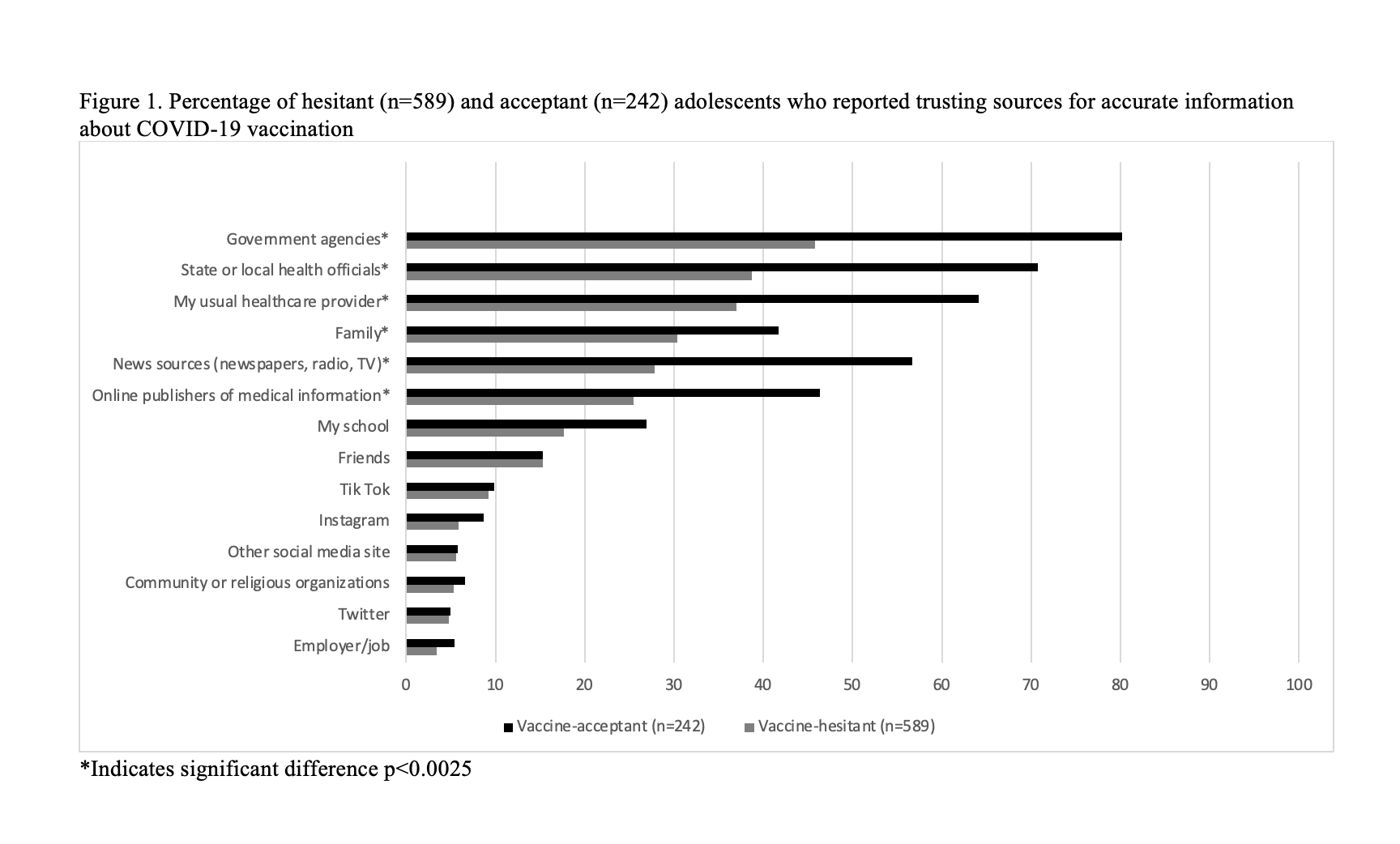
Most (n=589; 70.9%) adolescents were vaccine-hesitant, with increased hesitancy among those with lower levels of concern about COVID-19 infection and higher levels of concern about vaccine side effects. Among vaccine-hesitant adolescents, reasons for not intending to get vaccinated included wanting to wait for safety data and having parents who would make the decision. Vaccine-hesitant adolescents had a lower number of trusted information sources (M=2.75) compared to vaccine-acceptant adolescents (M=4.35). The top three sources of trusted information were government officials (45.8% of hesitant adolescents; 80.2% of acceptant adolescents), state/local health officials (38.7% of hesitant adolescents; 70.7% of acceptant adolescents), and usual healthcare provider (37.0% of hesitant adolescents; 64.1% of acceptant adolescents).
Conclusion(s):
We identified important differences between COVID-19 vaccine-accepting and vaccine-hesitant adolescents, which can inform communication with hesitant adolescents in terms of message content and dissemination channels. Targeting reasons for hesitancy by using theory-based messaging strategies to address them could prove to be an important next step for developing adolescent-facing communications.