Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 5: Epi/HSR Covid-19/Potpourri
797 - Prevalence of and factors associated with neonatal seizures in the United States.
Publication Number: 797.249
- MM
Mihir Mantena
Student
Pennsylvania State University
Timonium, Maryland, United States
Presenting Author(s)
Background:
Although prevalence varies by gestational age (GA), neonatal seizures are significantly influenced by various antenatal and intrapartum risk factors with an overall reported prevalence of 1 to 3 per 1000 live births. Advances in perinatal care with best care practices, and better diagnostic, and monitoring techniques have enabled accurate identification of clinical neonatal seizures in both preterm and term infants.
Objective:
To report recent national trends in the prevalence of neonatal seizures and to compare the associated maternal and infant risk factors among newborns with and without seizures during birth hospitalization.
Design/Methods:
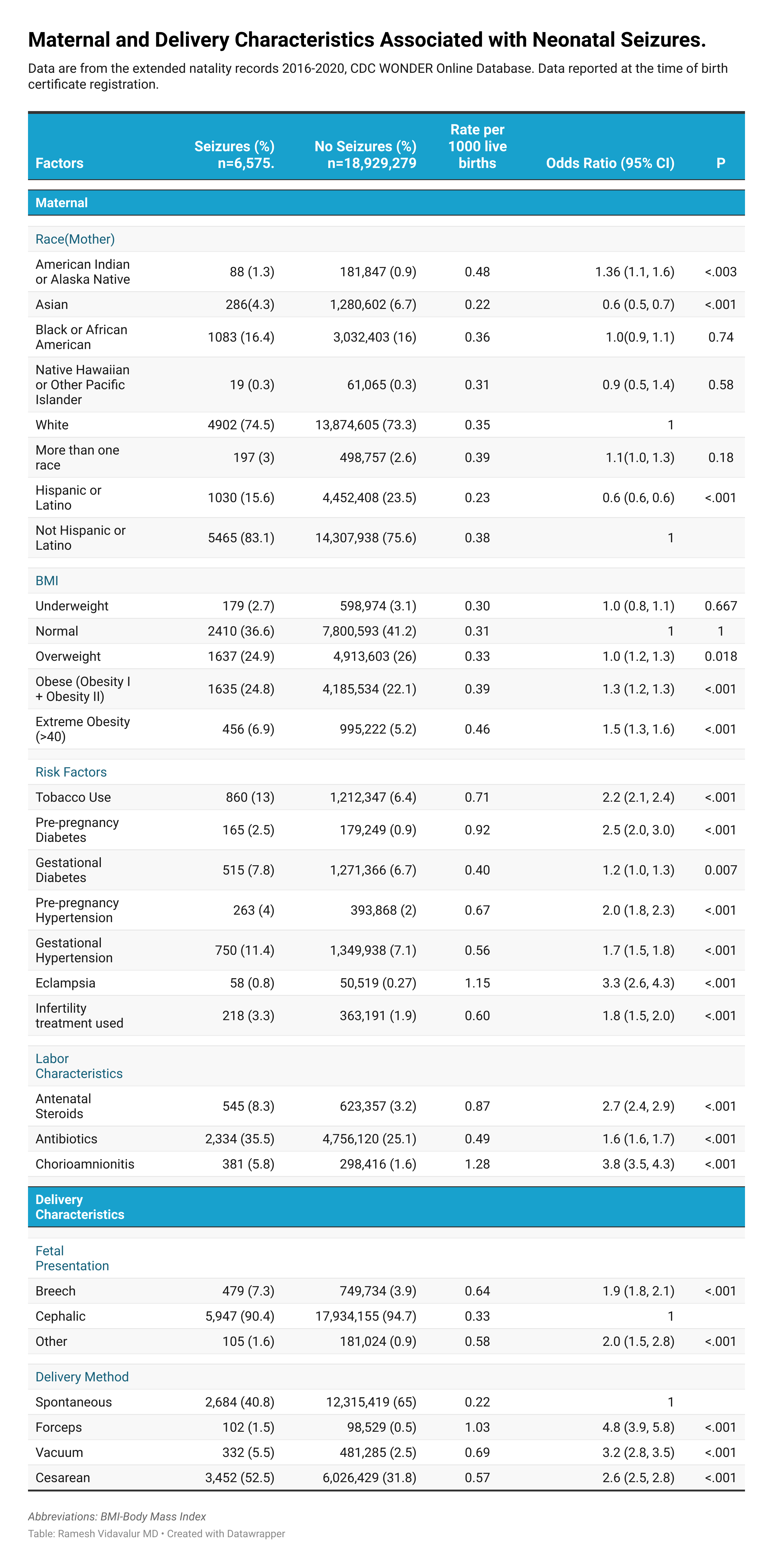
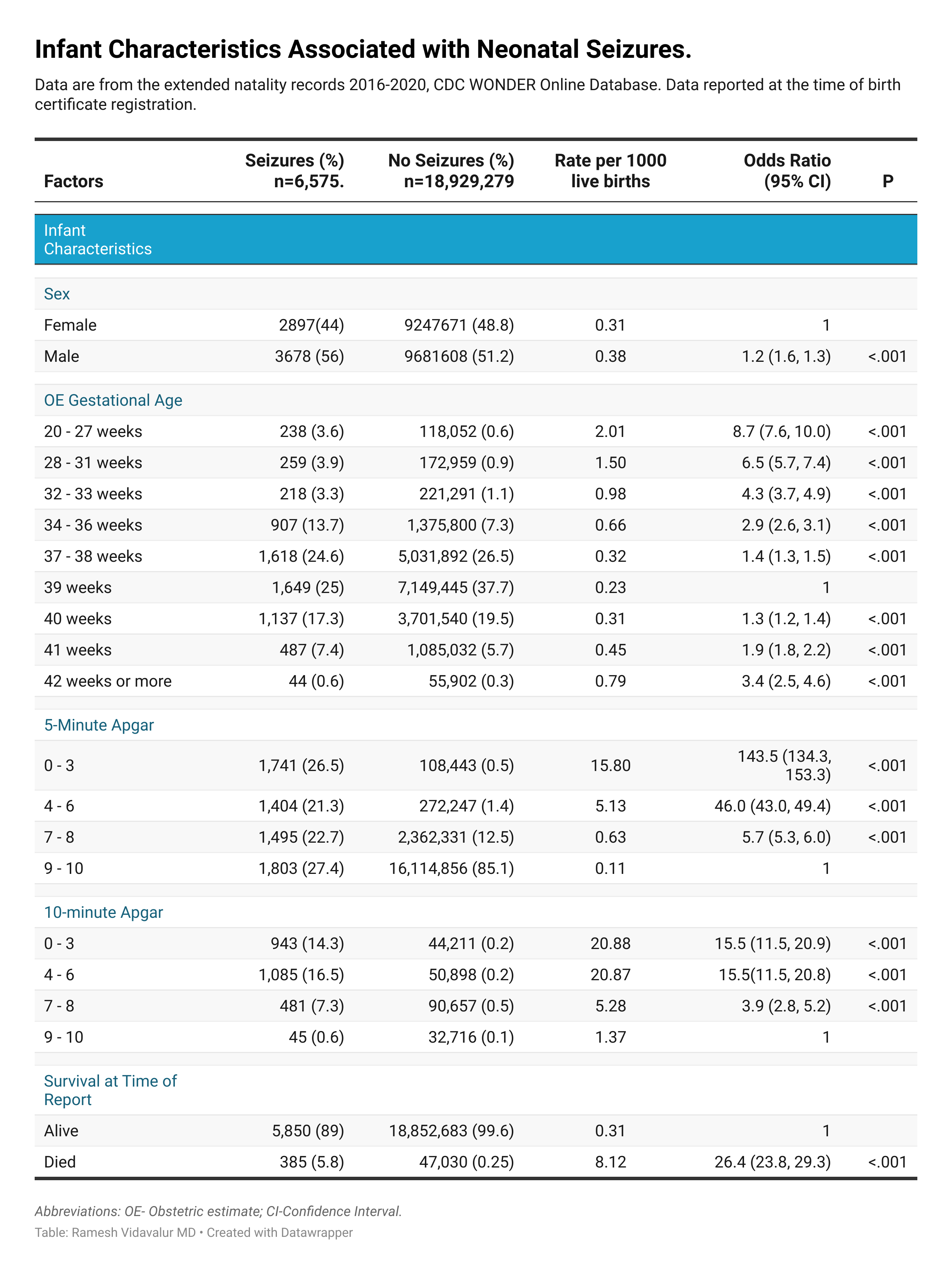
We used the US Centers for Disease Control and Prevention WONDER expanded natality database from 2016-2020 to extract maternal, delivery, and infant characteristics associated with neonatal seizures among all live births from detailed birth certificate data gathered by local state health departments. We used descriptive statistics to describe percentages, prevalence rates per 1000 live births, and bivariate analysis to determine odds ratios (OR) with 95% confidence intervals using PRISM software, version 9.4 (GraphPad Software). All P values were from 2-sided tests, and results were deemed statistically significant at P < .05.
Results:
From 2016 to 2020, among 18,935,854 birth hospitalizations, 6,575 (0.03%) newborns had seizures. Median state-level prevalence rate was 0.4 (IQR, 0.30, 0.7) per 1000 live births and no significant time trends (p=.85) were observed [Figure 1]. Strongest maternal risk factors for neonatal seizures include maternal chorioamnionitis (OR 3.8; 95% CI: 3.4, 4.2), exposure to antenatal steroids (OR 2.6; 95% CI: 2.4, 2.9), and use of assisted reproduction technology (OR 1.7; 95% CI: 1.5, 2) [Figure 2]. Seizure risk was highest in infants born at less than 28 weeks (OR 8.7; 95% CI: 7.6, 10.0), breech presentation (OR 1.9; 95% CI: 1.7, 2.1), 5-minute Apgar score < 7 (OR 46.2; 95% CI: 44.0, 48.0), and male sex (OR 1.2; 95% CI: 1.2, 1.3) [Figure 3]. Overall mortality rate was 5.8% ([95% CI: 5.2, 6.4]; OR 26.3 [95% CI: 23.7, 29.2], p< 0.001) in those who had seizures [Figure 3].
Conclusion(s):
This study identified several antenatal, intrapartum, and infant risk factors that were associated with an increased magnitude of risk for neonatal seizures. We observed a U-shaped distribution of seizure risk with gestational age at birth. Our summary findings strengthen the evidence base to offer better postnatal parental counseling, plan for clinical pharmacotherapy trials, and highlights the impact of higher seizure burden from associated risk factors..png)