Neonatal Nephrology/AKI
Neonatal Nephrology/AKI 1
221 - Renal Oxygenation in Critically Ill Preterm Neonates on Invasive and Non-Invasive Positive Pressure Ventilation
Publication Number: 221.242
Derek Gross (he/him/his)
Medical Student
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background:
Preterm neonates frequently require positive pressure ventilation (PPV) to support respiratory function during their NICU admission. Careful titration of mean airway pressure (MAP) is essential for these patients to avoid barotrauma and hemodynamic compromise that may lead to acute kidney injury (AKI). Near infrared spectroscopy (NIRS) monitoring has the potential to evaluate the effect of different MAPs by measuring renal regional tissue oxygenation (RrSO2).
Objective: We sought to determine if increases in MAP result in decreases in kidney oxygenation and to identify a MAP range that yields RrSO2 ≥ 50%.
Design/Methods: A retrospective analysis of MAP and renal regional tissue oxygenation (RrSO2) was performed on preterm neonates < 32 weeks’ gestation who were enrolled in a prospective NIRS monitoring study. INVOS NIRS sensors were placed on neonates within 48 hours of age and monitored RrSO2 every 5 seconds until 7 days of age. Hourly MAP recordings from chart review were compared to hourly averages of RrSO2 at the corresponding time points. Statistical analysis included linear and binomial mixed-effect models, Mann-Whitney U tests, and Fisher’s exact test.
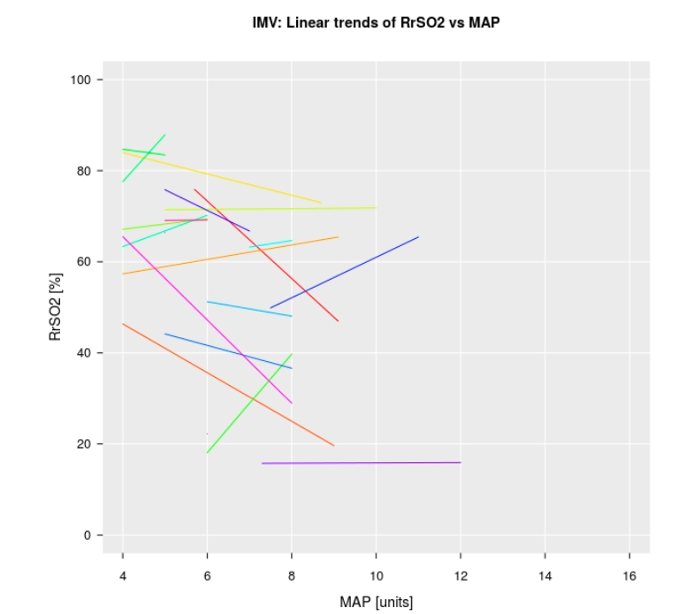
Results: Of the 35 neonate cohort, 18 received invasive mechanical ventilation (IMV) and 20 received noninvasive ventilation (NIV) between 2-7 days of age. The average gestational age and birth weight was lower for the IMV group compared to the NIV group. A 1 cmH2O increase in MAP is associated with a 0.53 percentage point (ppt) reduction in average RrSO2 in the IMV group (95% CI: 2.55 ppt reduction up to a 1.54 ppt increase; p = 0.61) and a 1.09 ppt reduction in the NIV group (95% CI: 2.99 ppt reduction up to a 0.88 ppt increase; p = 0.28). The odds ratio for an association between MAP and the odds of having RrSO2 ≥ 50% was 0.80 (95% CI: 0.63–1.04, p = 0.09) and 0.72 (95% CI: 0.53–0.99, p = 0.05) for the IMV and NIV groups, respectively.
Conclusion(s): In this pilot analysis, there was no consistent association between MAP and RrSO2 in both the IMV and NIV groups. These results highlight how the effect of MAP on kidney oxygenation is highly variable in premature neonates and demonstrates that NIRS monitoring may have a useful role in promoting kidney-mindful respiratory interventions. Further studies are needed to discern the mechanisms by which PPV affects kidney perfusion and oxygenation.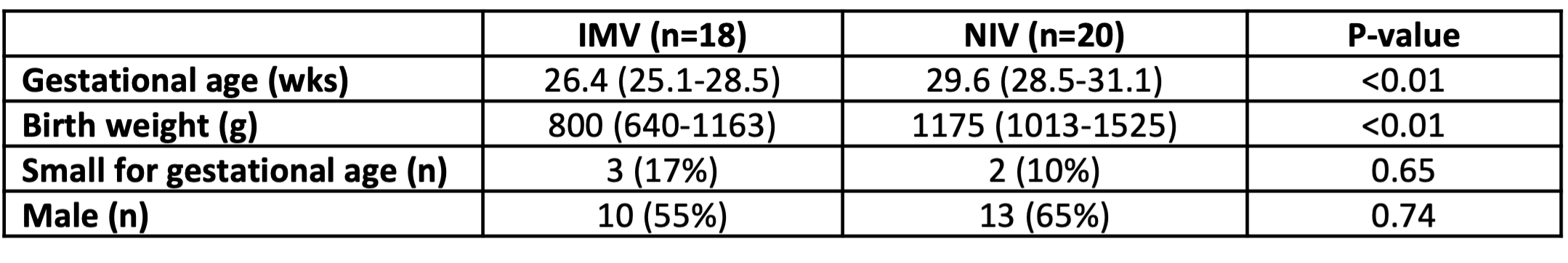
.png)
