Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 4: Epi/HSR Utilization, Cost, Outcomes
783 - Site-specific Costs for Extreme Preterm Care in Large Tertiary Level Canadian NICUs between the Years 2010 to 2021
Publication Number: 783.248
- TY
Telford Yeung, MD PhD
Neonatologist
University of Windsor
Windsor, Ontario, Canada
Presenting Author(s)
Background:
The Evidence-based Practice for Improving Quality (EPIQ) initiative is a Canadian quality improvement project that led to improved neonatal outcomes for infants born extremely preterm without significant increases in costs per day in neonatal intensive care; however, variation in outcomes and costs exist between neonatal units which have not been described from the perspective of the provincial public payor.
Objective: To quantify the variations in site-specific costs of NICU care for neonates < 28 weeks’ gestation admitted during the years 2010 to 2021 and correlate it with variations in outcomes.
Design/Methods:
We conducted a retrospective analysis of infants admitted after birth at < 28 weeks’ gestation in the Canadian Neonatal Network (CNN) sites between the years of 2010 and 2021. Sites that provided care for at least 50 infants per year during the study period in each gestational age group (23 to 27 completed gestational weeks) were included. Using a validated costing algorithm that assessed physician, nursing, respiratory therapy, diagnostic imaging, transfusions, procedural, medication and certain indirect costs, we calculated site and resource specific costs adjusted to 2017 Canadian dollars (CAD) using the Statistics Canada consumer price index.
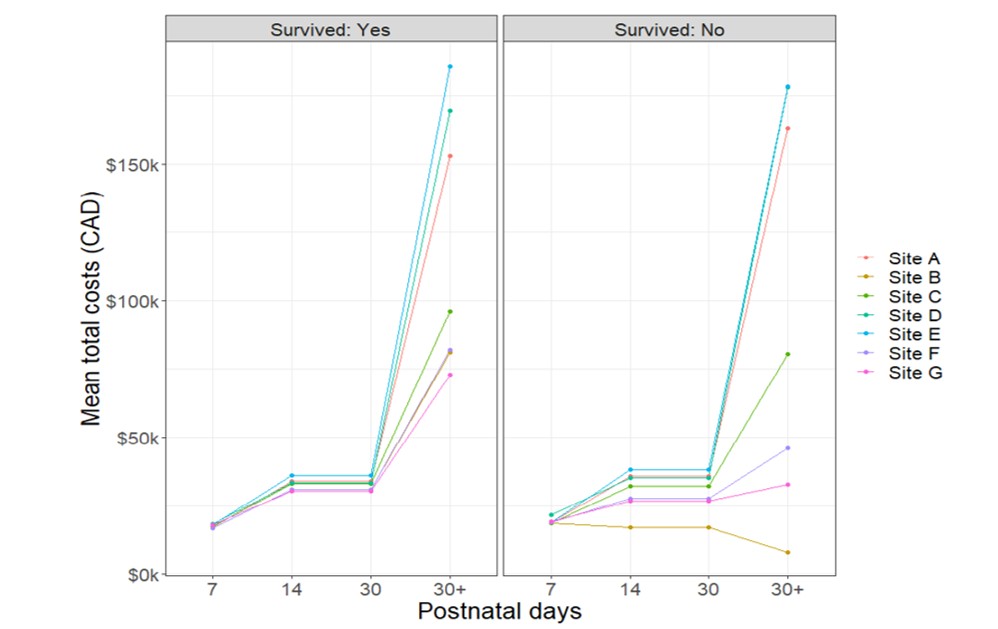
Results: We included seven sites in Canada that admitted a total of 8180 (range 841-1605) eligible neonates with a mean (standard deviation (SD)) gestation of 25.4 (1.3) weeks. Survival to discharge or transfer was 85.3% with a mean (SD) length of stay of 74.9 (46.4) days. The mean (SD) total costs per neonate was $116 021 (90 596) CAD, with survivors accounting for $126 393 (87 810) CAD and non-survivors accounting for $55 924 (82 890) CAD. Nursing care, respiratory support and indirect costs were the largest contributors to total costs (Table 1). Total and direct costs had greater variation among non-survivors compared to survivors (Figure 1); whereas, variation in costs between sites was the highest from day 30 of admission to discharge or transfer compared to the first 30 days of admission (Figure 2).
Conclusion(s): The costs of care for infants born extremely preterm varied between sites. Correlation between costs and outcomes may provide an important avenue for cost and outcome benchmarking.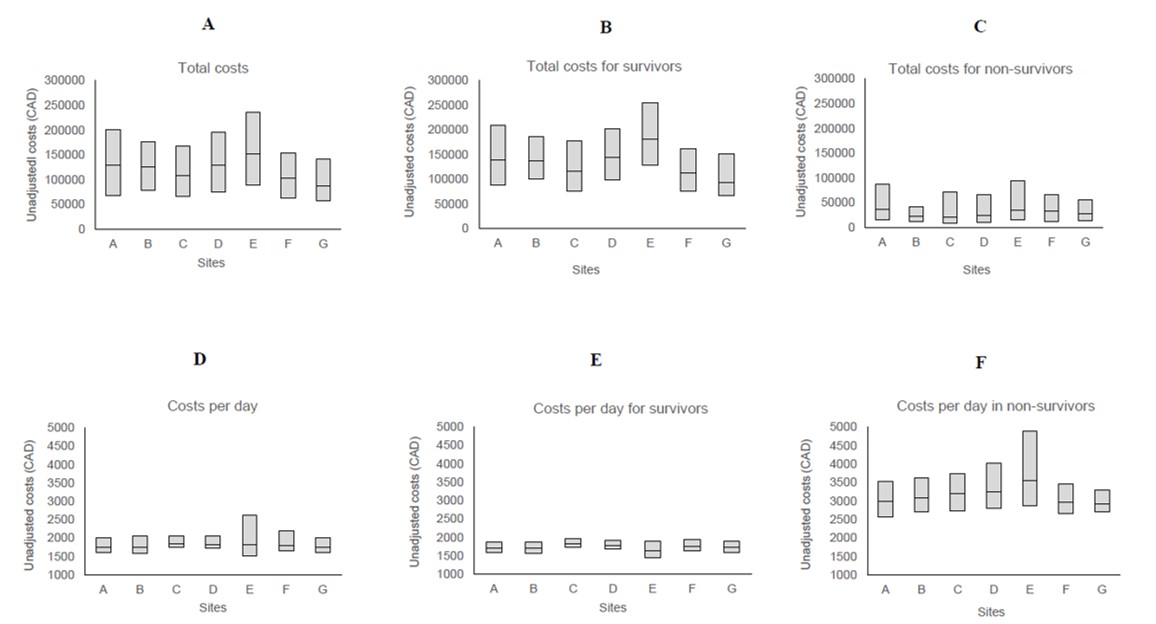
.jpg)
