Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 1: Bilirubin
114 - Early Onset Sepsis and Bilirubin Albumin Binding Affinity in Premature Infants
Publication Number: 114.238
- SA
SANJIV B. AMIN, MD, MS (he/him/his)
Professor
CHILDREN HOSPITAL OF MICHIGAN, CENTRAL MICHIGAN UNIVERSITY
Detroit, Michigan, United States
Presenting Author(s)
Background: Unbound bilirubin (UB), bilirubin not bound to albumin, crosses the intact blood brain barrier and the neuronal cell membrane, ultimately leading to neuronal injury. UB concentration depends on total serum bilirubin concentration (TSB), albumin concentration, and or bilirubin albumin binding affinity (K). In a previous study of premature infants, reserve albumin concentration, determined by dialysis with 14C-monoacetyl diamino diphenyl sulfone, was shown to decrease in the presence of sepsis, suggesting that sepsis may be associated with an increase in UB concentration. However, the association of sepsis with K and UB has not been well studied using direct measurement of UB in premature infants.
Objective:
To evaluate the effect of early-onset sepsis on K and UB concentration in premature infants.
Design/Methods:
We performed a prospective nested case control study involving < 32 weeks gestational age (GA) infants at birth. Infants with early-onset culture-positive sepsis (cases) were matched (1:1) on GA with infants without sepsis or histopathological chorioamnionitis (controls). Infants with asphyxia (Apgar score < 3 at 5 minutes), hemolysis (maternal and infant blood group mismatch with a positive indirect or direct coombs test), chromosomal disorders, cranio-facial malformations, or conjugated hyperbilirubinemia were excluded. TSB and UB were measured using the same aliquot of blood collected within 24 hours after birth and then twice daily during the first postnatal week. UB was measured by the modified peroxidase method. Serum albumin concentration was measured in individual subjects using the bromocresol green method. The UB, corresponding TSB, and serum albumin were used to calculate the K (L/μmol) using the law of mass action equation defined in literature.
Results:
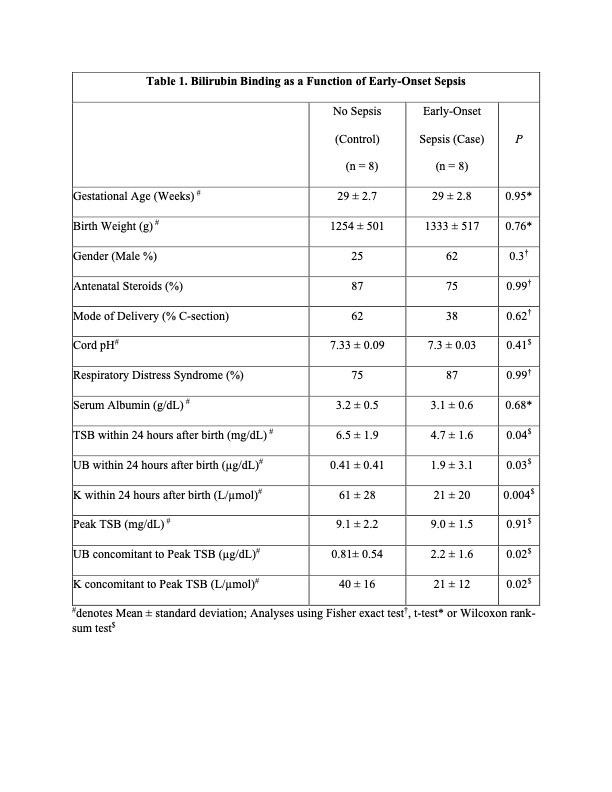
Nine premature infants were identified with early-onset sepsis of which 1 infant with asphyxia was excluded. A total of 16 infants (8 with culture proven sepsis and 8 control infants) were studied. There were no differences in clinical characteristics between the two groups (Table 1). Despite lower TSB, the UB was higher, and the K was lower in infants with sepsis compared to control infants in the first 24 hours following birth. Although there was no difference in peak TSB, the concomitant UB was higher and the K was lower among infants with sepsis compared to control infants (Table 1).
Conclusion(s):
Early-onset sepsis may be associated with a decrease in K and an increase in UB concentration. Premature infants with early-onset sepsis are at increased risk of bilirubin-induced neurotoxicity.