Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 2: Hematology
133 - The effect of transfusions on brain development do not vary by sex
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 133
Publication Number: 133.239
Publication Number: 133.239
Kendell German, University of Washington School of Medicine, Seattle, WA, United States; Thomas R. Wood, University of Washington School of Medicine, Seattle, WA, United States; Semsa Gogcu, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Patrick Heagerty, University of Washington, seattle, WA, United States; Dennis E.. Mayock, UWMC, Lake Forest Park, WA, United States; Bryan Comstock, University of Washington School of Medicine, Seattle, WA, United States; Mihai Puia-Dumitrescu, University of Washington School of Medicine, Seattle, WA, United States; Sarah E. Kolnik, University of Washington - Seattle Children's Hospital, Seattle, WA, United States; Ulrike Mietzsch, University of Washington School of Medicine, Seattle, WA, United States; Janessa Law, University of Washington, Seattle, WA, United States; Krystle Perez, University of Washington School of Medicine, Seattle, WA, United States; Gregory C. Valentine, University of Washington, Seattle, WA, United States; Theo K. Bammler, University of Washington, Seattle, WA, United States; Sandra Juul, Sandra Juul, Bellevue, WA, United States
Tommy R. Wood, MD, PhD (he/him/his)
Research Assistant Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: The majority of extremely preterm infants (EP) receive blood transfusions following birth. Transfusions are associated with expression of pro-inflammatory cytokines and adverse neurodevelopment.
Objective: We sought to evaluate the effect of infant sex on the interaction between hematocrit, transfusion volume, cytokines, MRI scores, and neurodevelopment in EP infants.
Design/Methods: In this post-hoc analysis of the Preterm Erythropoietin Neuroprotection Trial (PENUT), we evaluated all infants with serum cytokine (interleukin (IL)-6, IL-8, IL-10, interferon gamma (IFN-γ), tau, and tumor necrosis factor Alpha (TNF-α)) levels obtained at 0, 7, and 14 days, MRI Kidokoro score at 36 weeks postmenstrual age, and/or Bayley Scales of Infant Development (BSID III) at 24 months corrected age. The interactions between sex, transfusion volume, hematocrit, cytokines at 0-7 and 7-14 days, MRI, and/or BSID III scores were evaluated using generalized estimating equation (GEE) models adjusting for additional exposure risk factors experienced during the transfusion time period. To evaluate whether the effects were secondary to transfusion versus anemia, the association between the lowest hematocrit (Hct) and outcome measures was similarly evaluated.
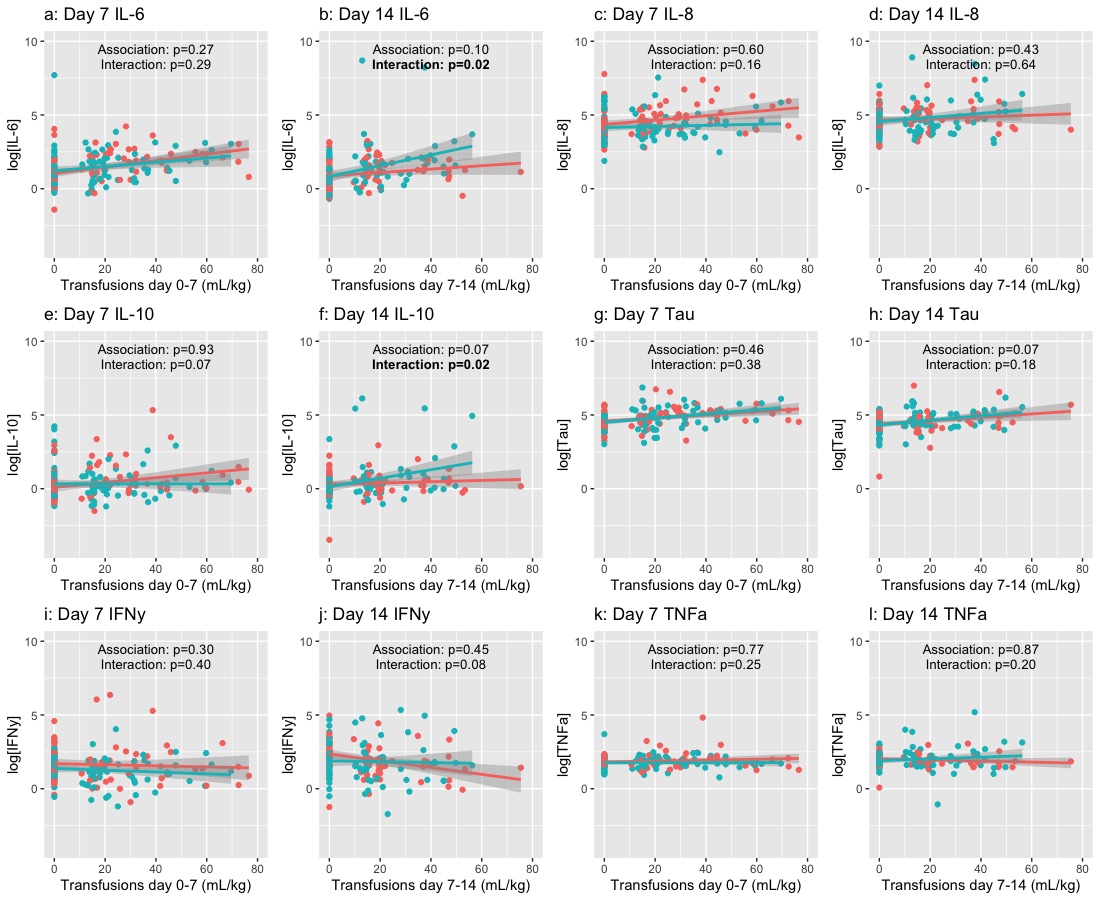
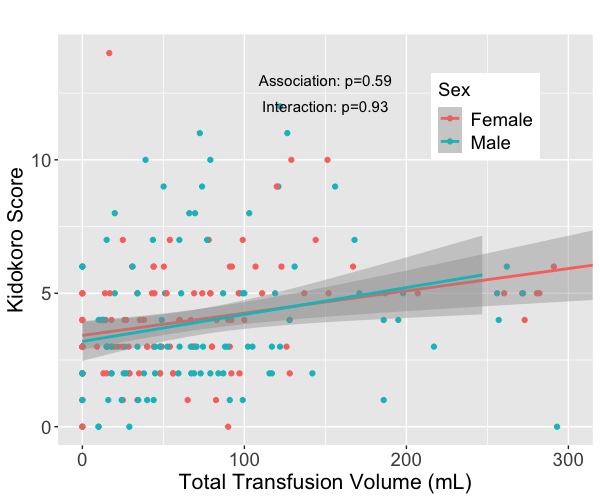
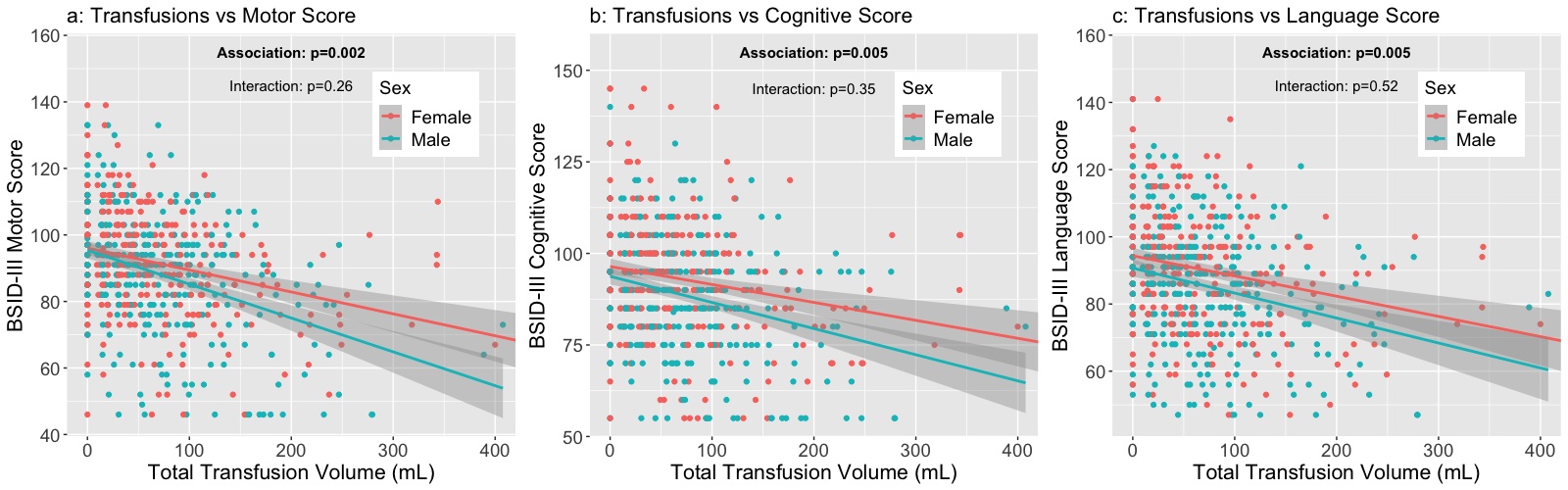
Results: 692 infants were included in the BSID III assessment, 220 infants had MRIs, and 184 and 164 infants were assessed with biomarkers at 0-7 and 7-14 days, respectively. A significant positive association was seen between transfusion and IL-6 and IFN-γ (Figure 1), with a negative association seen between MRI and BSID III scores (Figure 2). Infant sex modified the association between transfusion volume and IL-6 and IL-10 at 7-14 days but did not impact the association between transfusion volume and MRI score or BSID III subscales (Figure 3). The association between lowest Hct and BSID scores was significant only for the language domain (language p=0.046, motor p= 0.52, cognitive p= 0.55).
Conclusion(s): Blood transfusion volume, and not hematocrit, is associated with a significant increase in some inflammatory cytokines and worse 2-year neurodevelopmental outcomes. Infant sex impacts the short-term cytokine response to transfusion, however, this does not translate to differences in long-term outcomes, which are similarly negatively impacted by transfusion volume exposure regardless of sex.