Emergency Medicine: All Areas
Emergency Medicine 7
374 - Pediatric Electronic Sepsis Alert Performance in Rural Community Emergency Department
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 374
Publication Number: 374.211
Publication Number: 374.211
Nancy Clemens, Janet Weis Children's Hospital at Geisinger, Cogan Station, PA, United States; Megan Zelonis, Janet Weis Children's Hospital at Geisinger, Pittston, PA, United States; Sarah Alander, Geisinger Medical Center, Danville, PA, United States

Nancy Clemens, MD MS (she/her/hers)
Assistant Professor of Emergency Medicine and Pediatrics
Janet Weis Children's Hospital at Geisinger Medical Center
Cogan Station, Pennsylvania, United States
Presenting Author(s)
Background: Most children seek emergency care at community emergency departments (ED) and not at specialized pediatric hospital EDs. A two-stage electronic sepsis alert (ESA) screening tool has been shown to be highly sensitive and specific for recognizing sepsis when studied at an academic pediatric ED. It is unknown how pediatric electronic sepsis alerts perform in the community ED setting.
Objective: To evaluate the performance of a pediatric ESA in a rural community ED.
Design/Methods: We evaluated the test characteristics of a pediatric ESA by completing a single-site retrospective observational study in children presenting to a rural community ED between March 1, 2022 and August 31, 2022. We calculated sensitivity, specificity, positive and negative predictive value of the ESA, whether the patient was treated for sepsis in the ED, and whether sepsis was missed. A positive ESA (Table 1.) was defined as a high heart rate or low blood pressure that alerted the nurse to assess other risk factors and physical findings concerning for potential sepsis. We defined sepsis treatment as obtaining blood culture and receiving IV antibiotics and IV fluids. We defined missed sepsis as no ED sepsis treatment with subsequent ICU admission with IV antibiotics within 24 hours of admission.
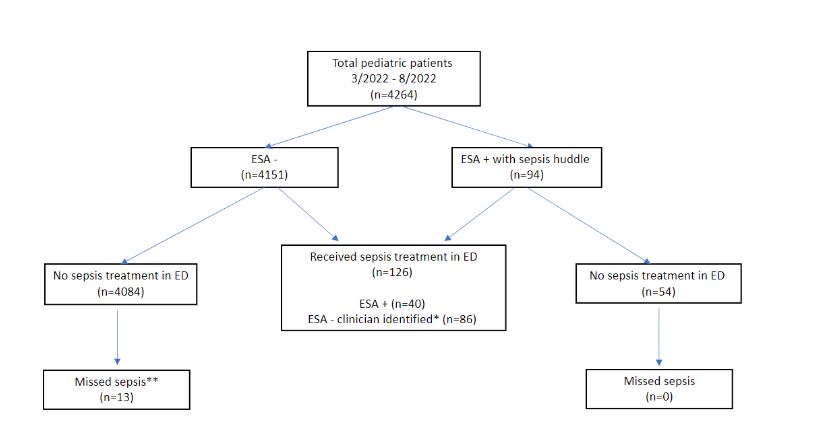
Results: 4264 children under 18 years presented to the ED over 6 months. Step one of the ESA triggered in 803 (18.8%). A sepsis huddle was documented in 94(2.2%), and 40 of those received sepsis treatment. Sepsis treatment was given to 86 children without a positive ESA. Sensitivity of ESA was 28.8% (95% CI: 21.4-37.1), specificity was 98.7% (95% CI: 98.3-99.0), positive predictive value 42.6% (95% CI: 33.8-51.8%), and negative predictive value 97.6% (95% CI: 97.4-97.9). There were 13 cases of missed sepsis; 8 had a positive step 1 which was dismissed and did not progress to the rest of the ESA (Figure 1.).
Conclusion(s): Use of the 2-stage ESA showed poor sensitivity in a community ED. The majority of missed sepsis cases had an initial alert due to abnormal vitals that did not progress to bedside huddle and treatment. Further research is required to determine how ESAs can be improved in community EDs to aid in identifying pediatric sepsis.
.jpg)