Neonatal Fetal Nutrition & Metabolism
Neonatal GI Physiology & NEC 4: Gut Health, Enteral Nutrition and Oral Feeding
84 - Influence of Mother’s Own Milk Compared to Pasteurized Donor Human Milk on Risk and Severity of Bronchopulmonary Dysplasia in Preterm Very Low Birth Weight Infants
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 84
Publication Number: 84.236
Publication Number: 84.236
Azam Siddiqui, Virginia Commonwealth University School of Medicine, Richmond, VA, United States; Judith Voynow, Children’s Hospital of Richmond at VCU, Richmond, VA, United States; Nayef Chahin, Children's Hospital of Richmond at VCU, Richmond, VA, United States; Allison Williams, Virginia Commonwealth University School of Medicine, Richmond, VA, United States; Karen D. Hendricks-Munoz, Virginia Commonwealth University School of Medicine, Richmond, VA, United States

Azam Siddiqui, MD (he/him/his)
Fellow
Virginia Commonwealth University School of Medicine
Richmond, Virginia, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is a common complication of preterm very low birth weight (VLBW) infants. MOM (mother’s own milk) contains a variety of nutritional and immunologic properties that can improve outcomes in preterm infants. PDHM (pasteurized donor human milk) is often used as an alternative when MOM is unavailable. The data on the influence of MOM and PDHM on BPD is limited.
Objective: To determine the influence of mother’s own milk (MOM) compared to pasteurized donor human milk (PDHM) on the risk and severity of bronchopulmonary dysplasia (BPD) in preterm very low birth weight infants.
Design/Methods: We performed a retrospective chart review of preterm (< 34 weeks) and very low birthweight (< 1500 grams) infants who were born at the Children’s Hospital of Richmond (CHoR) during the years 2019 to 2021. We collected demographic data. We collected data on type of nutrition received (MOM, PDHM, PF) and timing of exposure to MOM and PDHM. We collected outcome data including incidence/severity of BPD, incidence of NEC, incidence of IVH/PVL, incidence of ROP, incidence of sepsis/meningitis, mortality, weight gain, linear growth, and head growth. Data was analyzed using chi-square tests, linear regressions, and a multinomial logistic regression with p values < 0.05 considered significant.
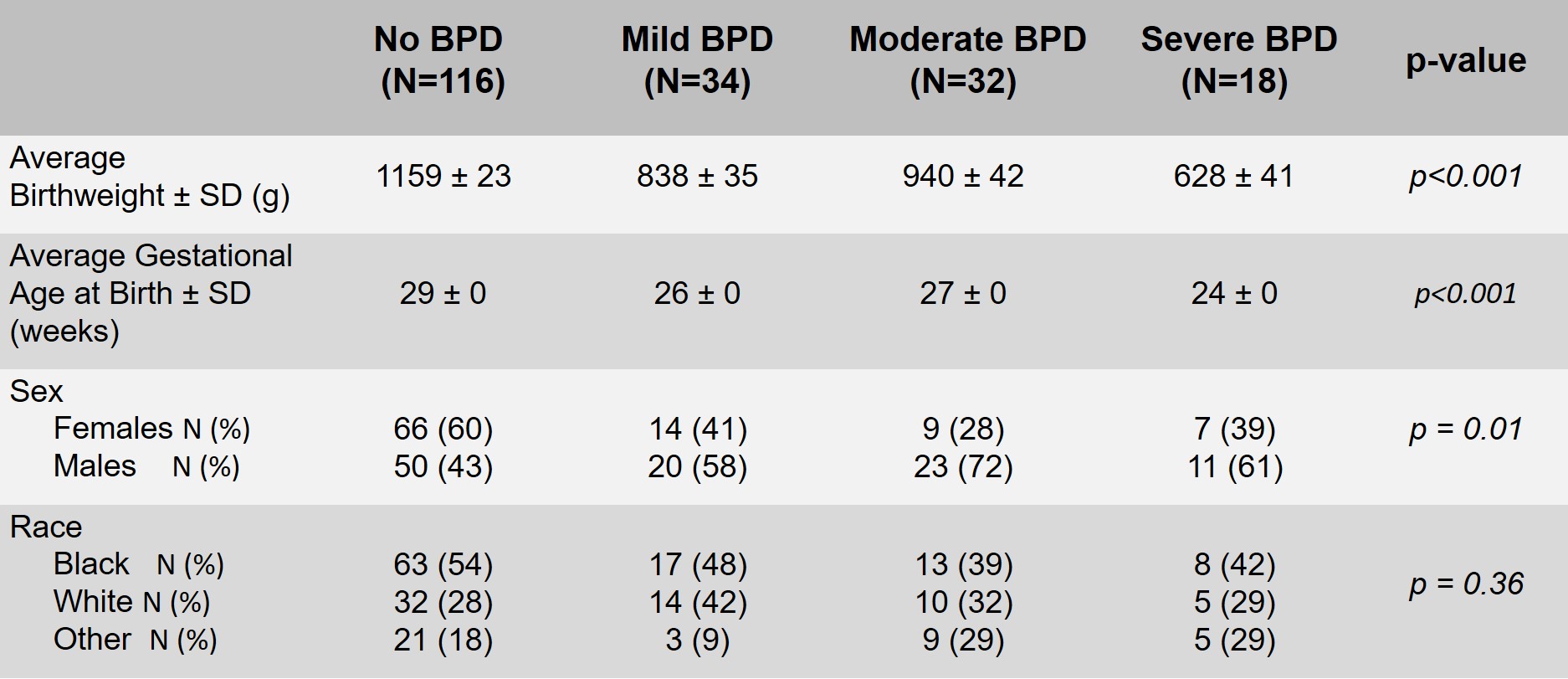
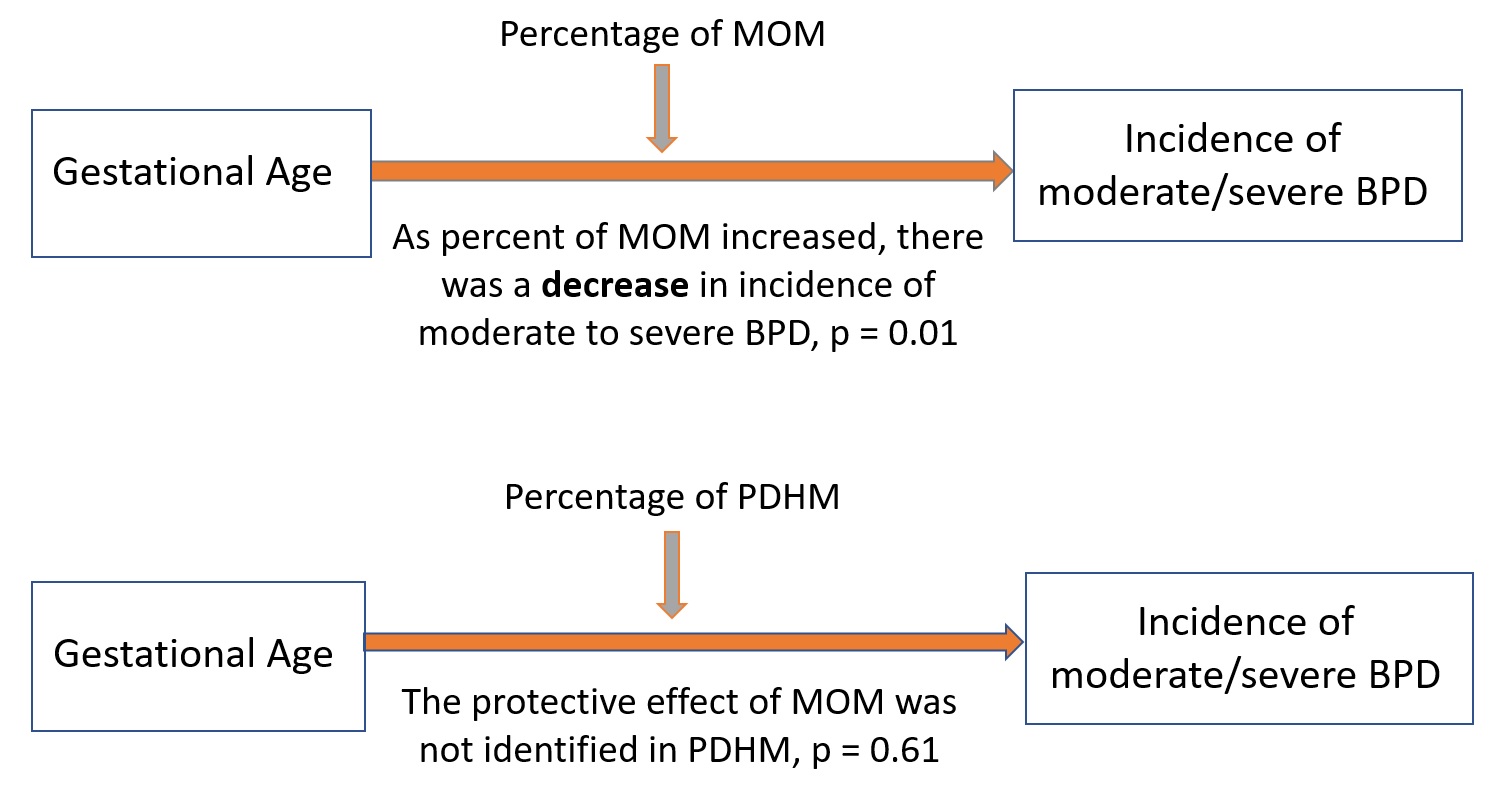
Results: There were a total of 236 infants that met inclusion criteria (gestational age < 34 weeks and birthweight < 1500 grams). There were 36 infants that were excluded. There were 200 infants included in our study of which 116 had no BPD, 34 had mild BPD, 32 had moderate BPD, and 18 had severe BPD. Infants exposed to MOM within the first three days and within the first seven days of life had lower incidences of moderate to severe BPD when compared to those who were not (p = 0.02, p = 0.04). Percentage of MOM and PDHM received was further analyzed as a moderator of the effect of gestational age on incidence of moderate to severe BPD. Percent of MOM received was a significant, negative moderator of incidence of BPD (p = 0.01, 95% CI [-0.14, -0.02]), such that as percent of MOM received increases, the effect of gestational age on severity of BPD decreases. In contrast, percent of PDHM received was not found to be a significant moderator of incidence of BPD (p = 0.61, 95% CI [2.28, 3.43]).
Conclusion(s): Our results show that greater percentage and earlier exposure to MOM is associated with decreased rates of moderate to severe BPD in preterm VLBW infants while greater percentage and earlier exposure to PDHM was not associated with lower rates of BPD.