Neonatal General
Neonatal General 5: COVID, Infections Diseases
696 - Low Rates of Transfusion-Transmitted Cytomegalovirus Infections Among Very Low Birthweight Neonates Receiving Leukoreduced-Only Red Blood Cells
Publication Number: 696.233

Rachel L. Brancamp, MD, MPA (she/her/hers)
Fellow
Vanderbilt University Medical Center
Nashville, Tennessee, United States
Presenting Author(s)
Background:
Preterm, very low birth weight (VLBW) infants have worse outcomes from cytomegalovirus (CMV) infection, which can be transmitted via blood transfusion. Available mitigation strategies include leukoreduction (LR) and selection of units from CMV seronegative donors; however, seronegative products have increased cost and sourcing difficulties. Previous studies have shown minimal risk of transfusion-transmitted CMV (TT-CMV) with LR-only products, but the appropriate mitigation strategy remains controversial.
Objective:
To determine the rate of TT-CMV in LR-only RBC transfusion.
Design/Methods:
We reviewed the electronic medical record (EMR) for all VLBW preterm neonates treated at Vanderbilt University Medical Center (VUMC) between November 2, 2017, and December 31, 2021, and who received red blood cell (RBC) transfusions. In patients with positive CMV serology, we interrogated the EMR to establish the course of infection and potential exposures. An independent pediatric infectious disease physician (SK) classified CMV infection as either congenital or acquired and determined the role of blood transfusion as a source. We determined the potential TT-CMV rate by comparing the number of cases where TT-CMV could not be excluded with the number of infants transfused. The impact of simultaneous platelet transfusion was also examined. Confidence intervals were calculated using a Poisson distribution, and differences in rates were analyzed using a chi-square test.
Results:
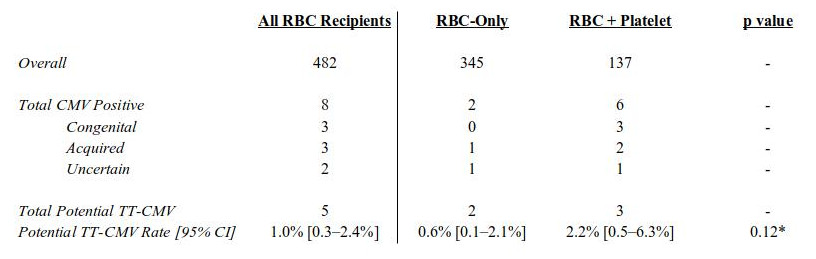
482 preterm, VLBW infants received LR-only RBC transfusions during the study period, 5 of whom had potential TT-CMV infection (Table 1). TT-CMV infection was not clinically suspected in any of these cases, but it could not be excluded. The potential TT-CMV rate was 1.0% (5/482, 95% CI = 0.3-2.4%). Concomitant platelet transfusion did not significantly alter this rate as compared to RBC-only transfusions (p = 0.12). The true rate of TT-CMV infection may be lower, or even zero, as other risk factors were present.
Conclusion(s):
There were no confirmed cases of TT-CMV in a 50-month retrospective review that included 482 preterm, VLBW infants receiving LR-only RBCs. In 5 cases of probable acquired CMV where TT-CMV could not be excluded, alternative sources of exposure, such as breastfeeding, were present. This is the largest study to date showing zero confirmed cases of TT-CMV in this patient population. Using LR-only blood products for transfusing VLBW infants is less costly and logistically easier than other mitigation strategies, especially given continued blood shortages during the Covid-19 pandemic.