Neonatal Nephrology/AKI
Neonatal Nephrology/AKI 1
220 - Recurrent neonatal acute kidney injury: Incidence, predictors, and outcomes in the neonatal intensive care unit
Publication Number: 220.242

Katherine G. Vincent, DNP, APRN, NNP-BC (she/her/hers)
Neonatal Nurse Practitioner
Medical University of South Carolina
Charleston, South Carolina, United States
Presenting Author(s)
Background: Acute kidney injury (AKI) occurs commonly in the neonatal intensive care unit (NICU) and is associated with increased morbidity and mortality. Neonates admitted to the NICU often have prolonged stays and may be subject to recurrent acute kidney injury (rAKI). Despite this very little is known about the incidence and impact of rAKI in the NICU.
Objective: We aimed to determine the incidence of rAKI, risks for rAKI, and the outcomes associated with rAKI in the NICU.
Design/Methods:
Single-center retrospective cohort study of neonates in the NICU 1/1/20-6/30/21. The neonatal modified Kidney Disease: Improving Global Outcomes criteria were used to define AKI. Baseline characteristics and potential AKI risk factors were compared between those with no AKI, single episode AKI (sAKI), and rAKI. Outcome measures included length of mechanical ventilation (LOV), length of hospitalization stay (LOS), mortality, and hypertension (HTN) at discharge. Multivariable linear and logistic regression models were used to examine associations between rAKI and outcomes, controlling for potential confounders.
Results:
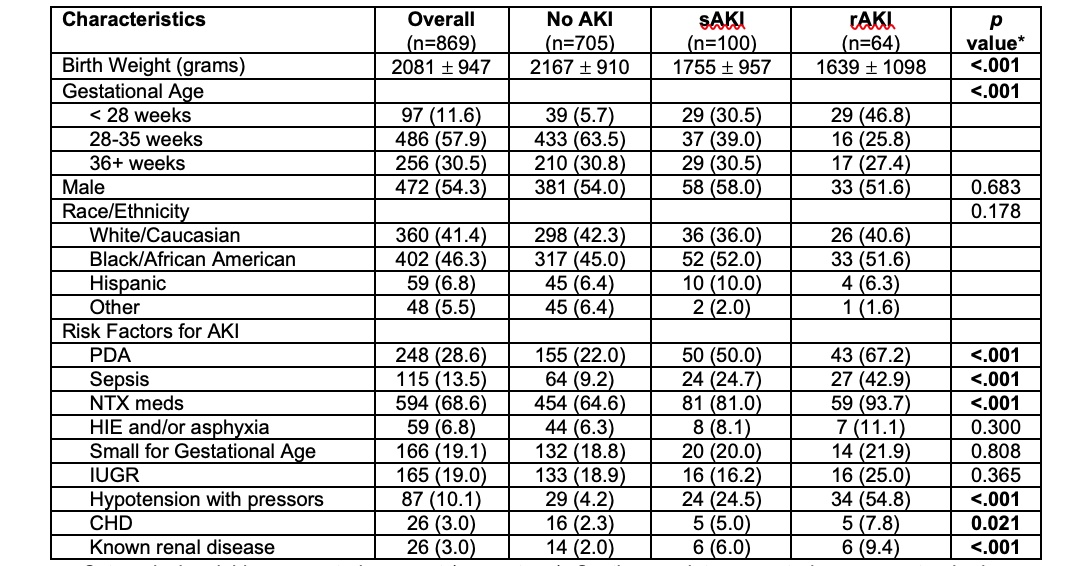
869 neonates were included in the study (705 (81%) no AKI, 100 (12%) sAKI, 64 (7%) rAKI). Neonates with rAKI had significantly lower birthweight (BW) and gestational age (GA) (Table 1). The distribution of AKI severity did not differ between those with sAKI and rAKI.
When examining potential confounders, neonates with rAKI more frequently had patent ductus arteriosus (PDA), sepsis, nephrotoxic medication exposure (NTX), hypotension, congenital heart disease (CHD), and renal disease than those with sAKI or no AKI (all p< 0.05, Table 1). Incidence of hypoxic ischemic encephalopathy, small for GA, and intrauterine growth restriction did not differ between groups.
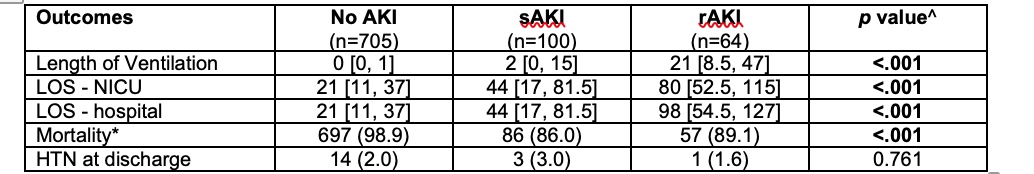
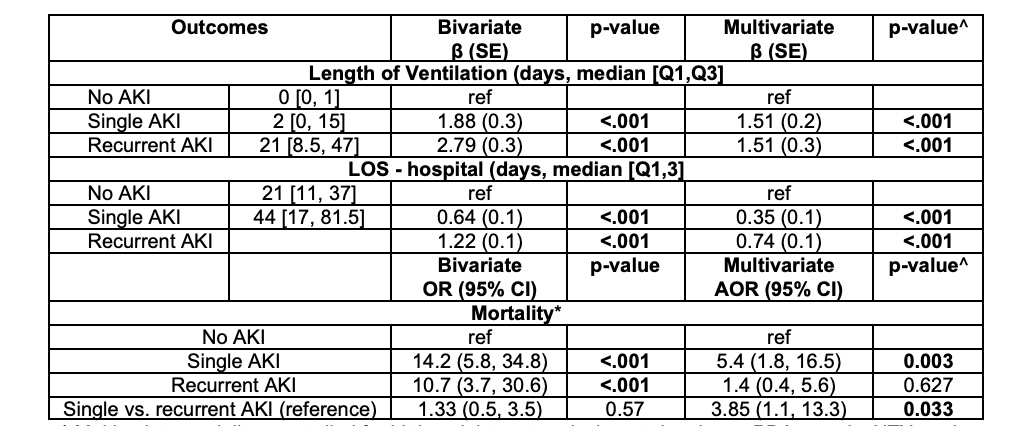
rAKI was associated with increased LOV, LOS, and length of NICU stay (Table 2). On multivariable analysis sAKI and rAKI were independently associated with increased LOV and LOS (Table 3). Mortality was highest in those with sAKI. sAKI was independently associated with almost 4x higher odds of mortality than those with rAKI.
Conclusion(s): In this single center cohort of all neonates in the NICU, lower BW and GA, as well as PDA, sepsis, NTX, hypotension, CHD, and renal disease are associated with rAKI. rAKI is independently associated with LOV and LOS suggesting rAKI is clinically important and warrants special attention and further study.