Breastfeeding/Human Milk
Breastfeeding/Human Milk 4: Breastfeeding and Milk Provision
35 - Breastfeeding at discharge after supplementation in the first 24 hours of life
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 35
Publication Number: 35.202
Publication Number: 35.202
Mohammed Al-Nahar, Michigan State University College of Human Medicine, Grand Blanc, MI, United States; Igbagbosanmi O. Oredein, Michigan State University College of Human Medicine, Grand Blanc, MI, United States; Nathalee Harris, Hurley Medical Center, Montrose, MI, United States; Navin Kumar, Michigan State University College of Human Medicine, Grand Blanc, MI, United States
.jpg)
Mohammed Al-Nahar, MD (he/him/his)
Resident Physician
Michigan State University College of Human Medicine
Grand Blanc, Michigan, United States
Presenting Author(s)
Background: Formula supplementation of newborns whose mothers intend to breastfeed can happen as early as their 1st feeding or later on during the stay in the well-baby nursery. The volumes that are supplemented in these early postpartum days are usually not correlating with the natural breast milk production (estimated range on day 1: 2-10 ml/feed).
Objective: Whether volumes per kg birth weight (BW) and other supplementation characteristics, in the 1st 24 hours of life (HOL) impacts the rate of “Breastfeeding at discharge” (BFAD) has not been well quantified and was investigated herein.
Design/Methods: We conducted a single-center retrospective chart review of 3102 breastfeeding infants born from March 2018 to March 2021 at GA ≥ 35 weeks and supplemented in the 1st 24 HOL. Infants were categorized into two groups based on the feeding documentation at discharge of either a) breastfeeding (BFAD), or b) formula feeding (FFAD). Four characteristics of supplementation [timing, type (expressed breast milk (EBM) or formula), rate and volume in ml/kg per feed] were correlated with BFAD.
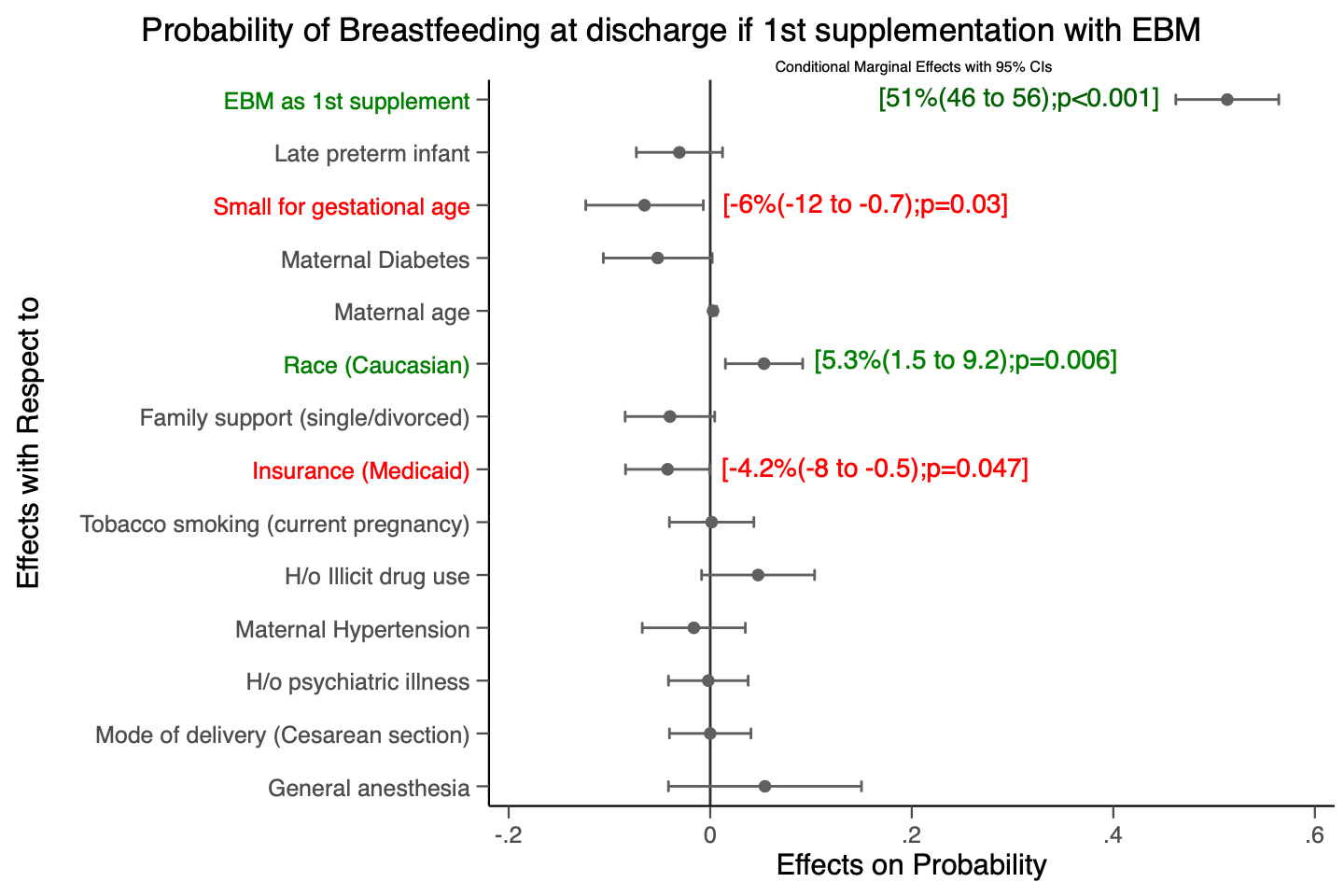
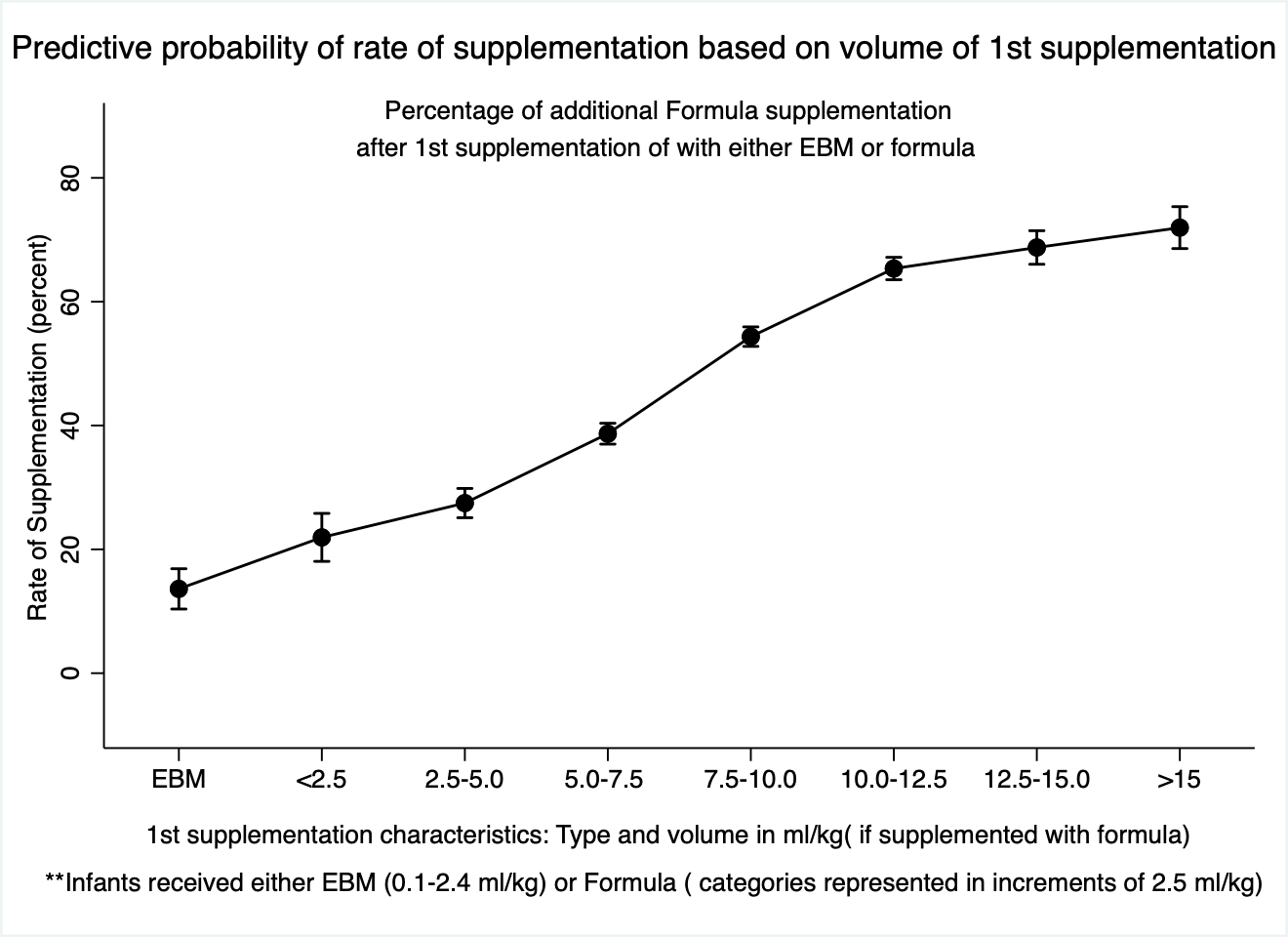
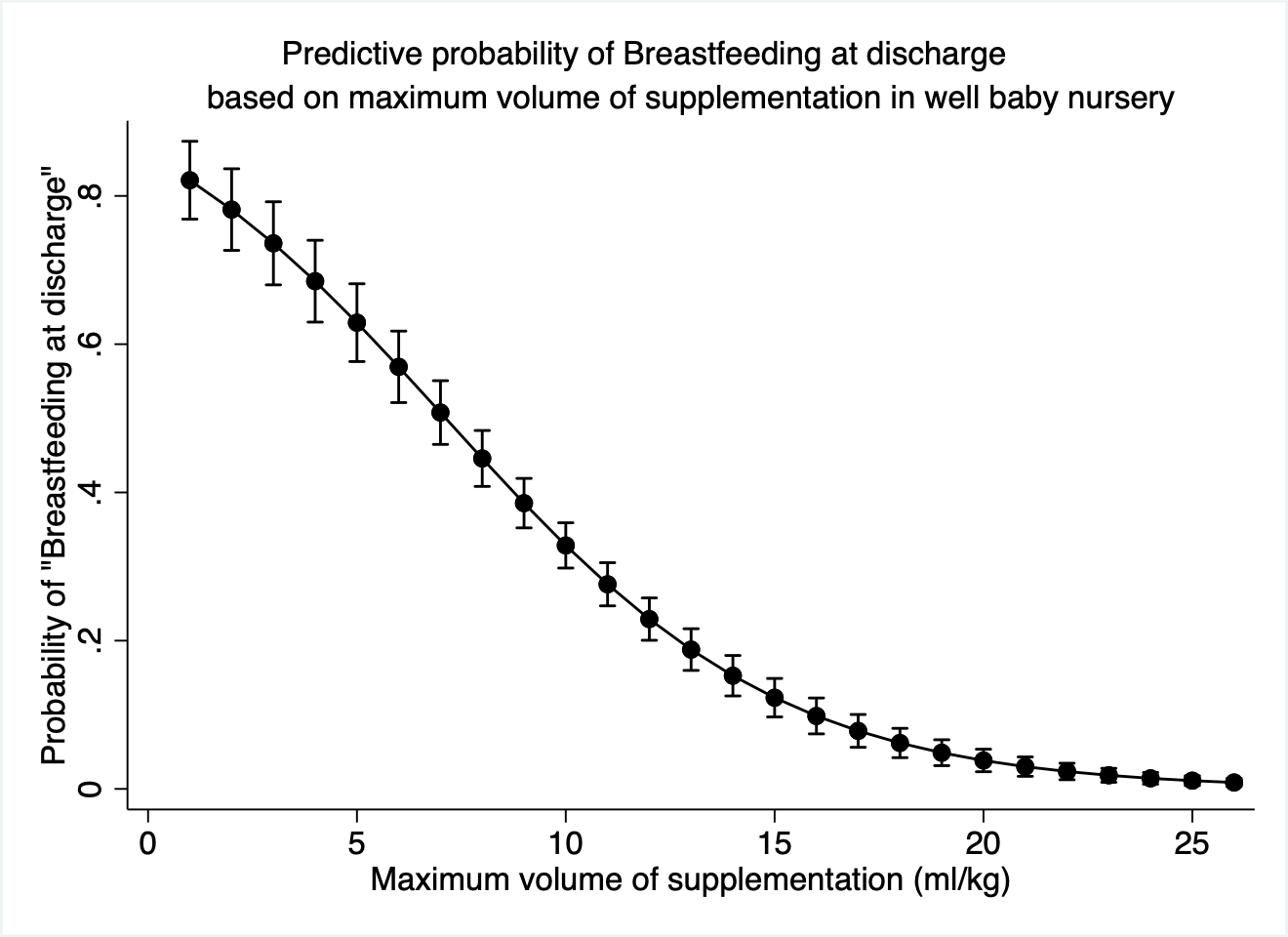
Results: 1031 (33.2%) infants were BFAD. Odds of BFAD increased by 2.8% (95% CI [.022, .035]) for each additional hour of supplementation time from birth. 223 (7.2%) were supplemented at least once with EBM. Even one EBM supplementation was associated with higher odds of BFAD [OR = 9.8, 95% CI 7.2-13.3; p< 0.001] (Figure 1). Linear regression analysis indicated a 4.5% increase in subsequent rates of supplementation with each 1 ml/kg increment in volume of the 1st supplementation [F (1, 3082) = 1883.43, R2 = .37, β = 0.61, P</span>< 0.001) (Figure 2). Receiver operator curve analysis showed that supplementation rates of ≤35.1% were predictive of BFAD [AUC 0.85 (0.84-0.86); Sn 74.2; Sp 80.1; p< 0.001]. Infants with rates < 35% were included in the final multiple logistic regression to analyze the impact of maximum volume of supplementation. Our analysis revealed an average 4.2% (3.6-4.7) drop in the predictive probability of BFAD with each unit increase from 2-15 ml/kg. (Figure 3).
Conclusion(s): Breastfeeding at discharge is negatively associated with early and higher supplementation volumes in relation to BW. These feeding patterns often tend to deviate from the normal breastfeeding volumes observed in the immediate postpartum phase. Early formula supplementation with these non-physiological volumes may be an important factor associated with lower breastfeeding rates at discharge, as they can potentially discourage mothers to continue breastfeeding.