Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 5: Epi/HSR Covid-19/Potpourri
795 - Impact of COVID-19 on parents, families and children born very preterm in California
Publication Number: 795.249

Susan R. Hintz, MD, MS (she/her/hers)
Professor
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background:
The impact of COVID on health care continues to unfold, particularly for children with special healthcare needs and their families. The extent to which the pandemic has added to the anxiety, stress and trauma experienced by parents, and to challenges in community supports and child health is not known.
Objective:
Among infants < 30 weeks EGA in participating California NICUs and high-risk infant follow up (HRIF) clinics, to characterize impacts of the early COVID period on 1) parental stress in NICU and post-discharge, 2) community services and resource challenges, and 3) perceived adverse child health effects.
Design/Methods:
A multilevel survey study of parents of infants born 3/1 to 8/31/20, < 30 weeks EGA, in participating California Perinatal Quality Care Collaborative (CPQCC) NICUs, survived to discharge, and referred to linked CPQCC California Children’s Services (CCS) HRIF clinics. The study was reviewed by site IRBs, and consents obtained. Survey was administered by emailed RedCap link, or phone or in-person. The 44-question survey included Likert scale, yes/no, multi-part, and open-ended response types, and had to be completed at 4-12 months corrected age. Survey data were linked to CPQCC NICU and HRIF datasets. We tested associations of a priori selected sociodemographic and neonatal characteristics with outcomes combining query scores.
Results:
A total of 148 parents consented (19 sites, N per site=2-38) of 255 eligible; 78 completed surveys. Cohort characteristics (Tab 1) show most had private insurance, and were without major neonatal morbidity. Responses (Tab 2) showed high rates of reported stress during the NICU stay due to COVID-related concerns. In open-ended queries (not shown), parents reported multiple actions associated with stress reduction in the NICU including bedside cameras, primary RN, communication. Parents experienced high rates of anxiety/trauma and resource/access challenges in the post-discharge period; 1 in 6 reported adverse child health impact due to COVID (Tab 2). Combined outcomes (Tab 3) demonstrate overall high parent stress due to COVID, but high perceived NICU support; outcomes scores in highest quartile were not associated with characteristics explored.
Conclusion(s):
Parents of infants < 30 weeks born in the early pandemic report high stress, anxiety and trauma due to COVID in the NICU and post-discharge, community resource/access challenges, and concerns for adverse health impact. These data set the stage for broader, statewide parent input to further elucidate stressors and valued outcomes, leading to NICU-to-community family-focused interventions.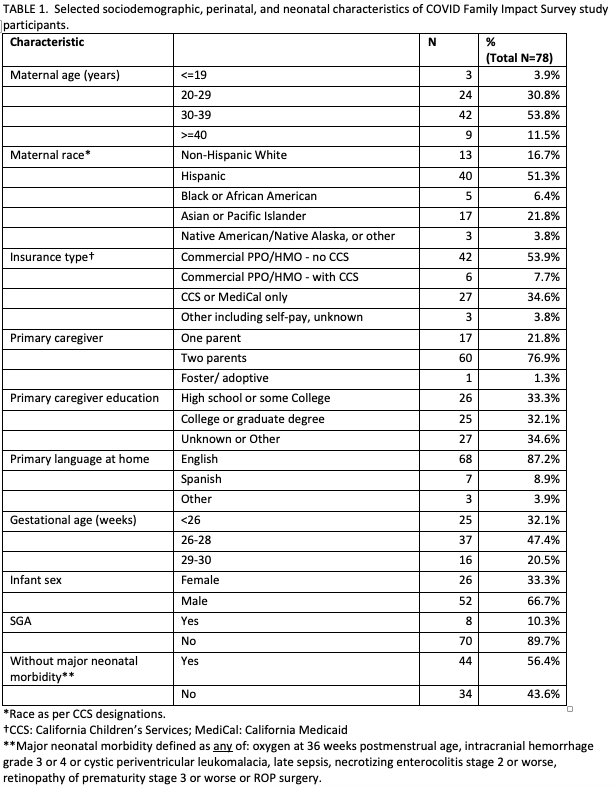
.png)
.png)
