Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 3: Gut Health Clinical Research
70 - Osmolality of Enteric Medications on Preterm Intestinal Enterocyte Viability
Publication Number: 70.235
- CM
Cydney Meyer, MD (she/her/hers)
Assistant Professor
UT Houston
Houston, Texas, United States
Presenting Author(s)
Background:
Necrotizing enterocolitis (NEC) is a dysregulated inflammatory response within the nascent intestine in which increases in cytokine and toll-like receptor (TLR) 4 expression precede clinical NEC. NEC is believed to manifest as a consequence of a variety of stimuli (intestinal immaturity, exposure to formula, hypoxia). Fluctuations in intestinal osmolality can adversely impact the neonatal intestine, but the role of enteric osmolality and the development of NEC is controversial. In 1976 the American Academy of Pediatrics (AAP) recommended a maximum 400 mOsm/mL in feeds for “normal infants”. Unfortunately, recent sampling of drugs used in infants demonstrates most are overwhelmingly hypertonic. Furthermore, the impact of pharmaceuticals on preterm intestinal tissues has not been assessed.
Objective:
We hypothesize increasing osmolality of drugs is associated with increased TLR and inflammatory cytokine expression, decreased metabolic activity, and decreased viability.
Design/Methods:
Osmolality of neonatal enteric drugs were measured. Fetal intestinal enterocytes (FHS-int74) were incubated for 3 hours at 1:10 dilutions of drugs with mannitol (non-absorbable sugar) and PBS used as controls. Expression of TLR-4, TLR-2, IL-6, IL-8, IL-1β, and TNF-α mRNA was determined by real-time PCR (qRT-PCR) with results normalized to 18s mRNA. Metabolic activity was assessed via 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) tetrazolium reduction (MTT) colorimetric assay and apoptotic activity via terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay. Results were analyzed via linear regression.
Results:
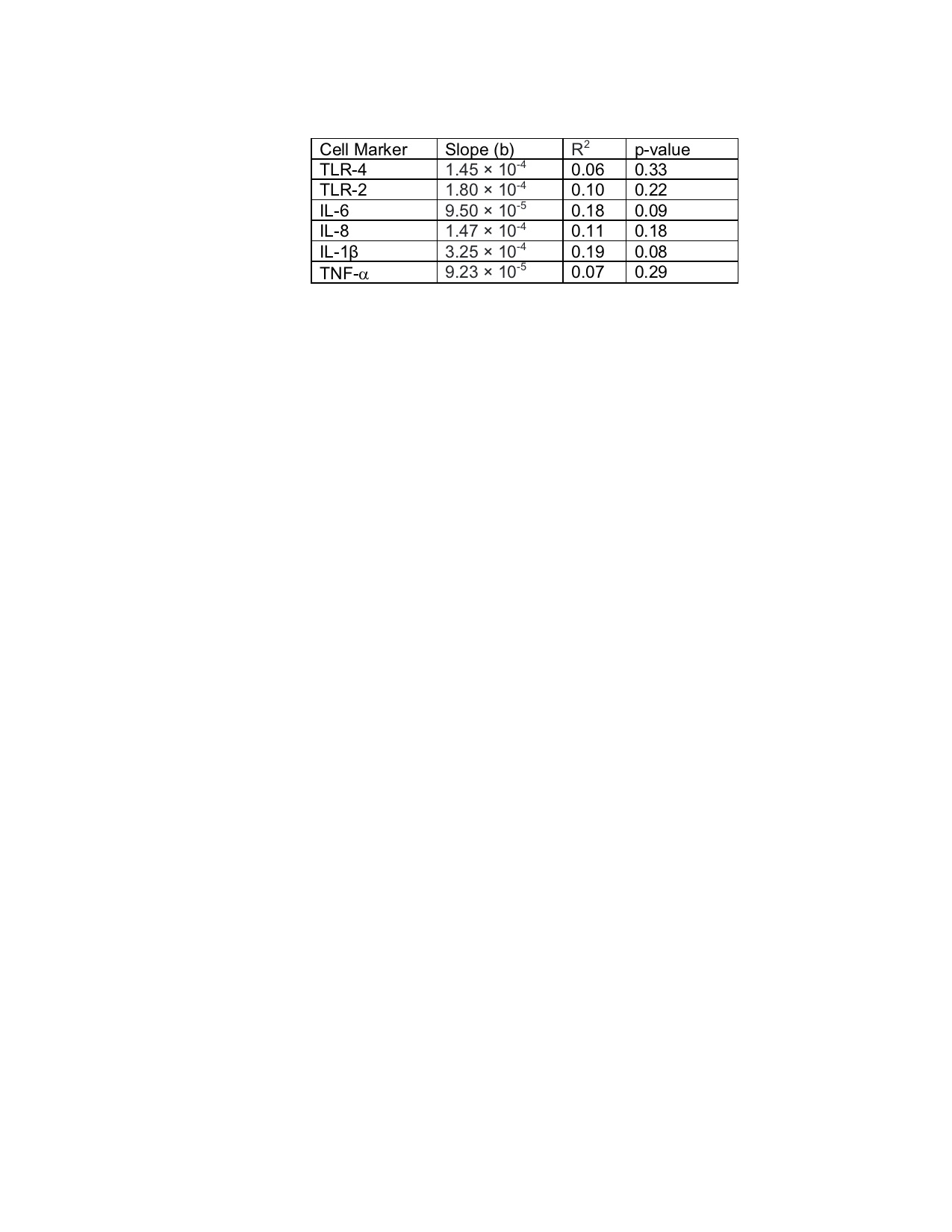
34 common NICU enteric drugs were measured: 8 (24%) measured < 500 mOsm/kg (within the AAP guidelines for enteric feeds). The remaining 8% (n=3) measured 500-1000 mOsm/kg, 38% (n=13) between 1000-4000 mOsm/kg, and 29% (n=10) >5000 mOsm/kg. Despite an excessively hypertonic cohort, no correlation between drug osmolality and TLR-4, TLR-2, or cytokines was observed (Table 1). Osmolality was also not correlated with enterocyte metabolic activity (b=6.52 × 10-6 , R2= 0.05, p= 0.34) or apoptosis grossly.
Conclusion(s):
The majority of measured enteric drugs are hyperosmolar, with most greater than AAP recommendations for feeds. Nonetheless, no correlation was observed between osmolality and expression of measured TLRs or cytokine expression, metabolic activity, or apoptotic activity. As dilutions of 1:10 are higher than expected in the neonatal intestines, our results suggest it is unlikely that osmotic stress alone contributes to increased intestinal inflammation leading to NEC.