Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 2: Hematology
131 - Cord blood reticulocyte hemoglobin content as a marker of iron deficiency at birth
Publication Number: 131.239

Geetika Kennady, MD
Neonatologist
Nemours Children's Health/ Thomas Jefferson University Hospital
Swedesboro, New Jersey, United States
Presenting Author(s)
Background:
Iron deficiency (ID) during fetal life and early infancy, even in the absence of anemia, is associated with neurocognitive impairment. It is crucial to identify infants who are iron deficient at birth. Up to 17% of the preterm infants are reported to be iron deficient at birth. The risk factors for IDA in infants include small for gestational age (SGA), prematurity, maternal history of placental insufficiency, iron deficiency, diabetes, obesity, smoking, alcohol ingestion, and intrapartum hemorrhage. About 8.9% of these high risk infants are ID at birth. Reticulocyte hemoglobin content (Ret-He) is an early indicator of ID.
Objective:
We aim to determine the prevalence of low Ret-He in umbilical cord blood and its utility in diagnosing ID at birth.
Design/Methods:
In a prospective cohort study, cord blood samples were collected from term and preterm infants after informed consents from the parents. Complete blood count (CBC), Ret-He, serum iron, total iron binding capacity (TIBC), transferrin saturation (TS) and ferritin was determined in the cord blood. Low Ret-He was defined as ≤ 27.4pg. Iron deficiency was defined as serum iron < 100 mcg/dL, TS < 30% and serum ferritin < 50 ng/ml.
Results:
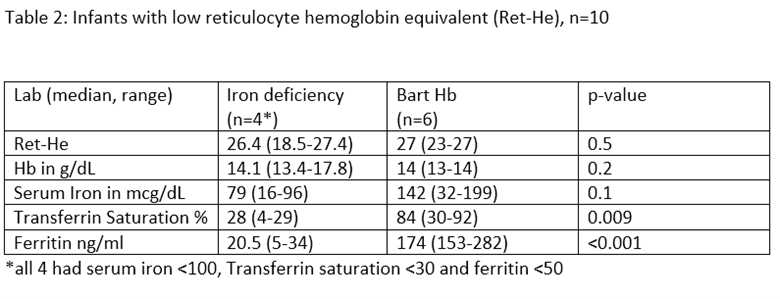
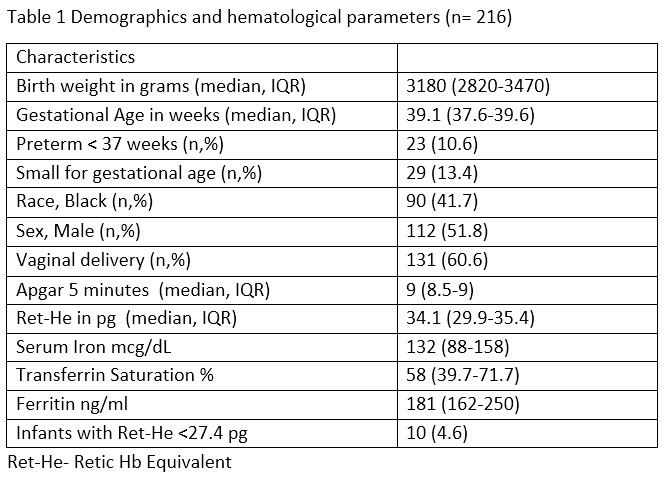
A total of 244 infants were enrolled and cord blood samples were collected. Ret-He was determined in 216 cord blood samples. The demographic characteristics are depicted in table 1. 10.6% of infants were preterm and 13.4% SGA. The median (IQR) Ret-He was 34.1 pg (29.9-35.1). Ten infants (4.6%) had low Ret-He at birth. Six of these infants were positive for Hb Barts (alpha thalassemia trait) and none of them had iron deficiency. Four infants had low RET-He with negative Hb Barts, all of them had biochemical evidence of ID. In the iron deficiency group, median hemoglobin (range) was 14.1 g/dL (13.4-17.8), median serum iron was 79 mcg/dL (16-96), median ferritin was 20.5 ng/ml (5-34) and median TS was 28% (4-29). All ID infants were born to mothers with anemia.
Conclusion(s):
At birth, 4.6% of the infants had low Ret-He. Infants with low Ret-He had either alpha thalassemia trait or ID. Ret-He in cord blood in the absence of Hb Barts is a potential marker of ID at birth. Infants born to mothers with anemia are at high risk for ID. Cord blood Ret-He can potentially be used to identify iron deficient infant at birth if our findings are confirmed in a larger study.