Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 4: Epi/HSR Utilization, Cost, Outcomes
781 - Survey on NICU Managers’ Perception of Organizational Challenges in the Neonatal Intensive Care Unit (NICU)
Publication Number: 781.248

Carla Herman (she/her/hers)
Medical Student
McGill University Faculty of Medicine and Health Sciences
Montreal, Quebec, Canada
Presenting Author(s)
Background: Each year, 15,000 critically ill neonates require specialized care that is offered in only 32 tertiary neonatal intensive care units (NICUs) in Canada. Although regionalization of perinatal care has improved care, staffing and bed capacity remain finite resources in a publicly funded healthcare system.
Objective: To explore neonatal managers’ perceptions of organizational challenges, namely nurse-to-patient ratios and unit bed occupancy, in Canadian NICUs.
Design/Methods: This was a web-based cross-sectional survey, consisting of 20 questions pertaining to the determinants of resource allocation, the ascertainment of high occupancy state, the different challenges and mitigation strategies implemented during periods of high unit acuity. The survey was designed following the CHERRIES guidelines and was critically reviewed through a two-round validation process. It was then sent by e-mail to the unit manager of all Canadian Level-3 NICUs between August and November 2022, who were invited to respond based on their practice in 2021. The analysis was conducted using descriptive statistics.
Results:
24 managers (75%) completed the survey.
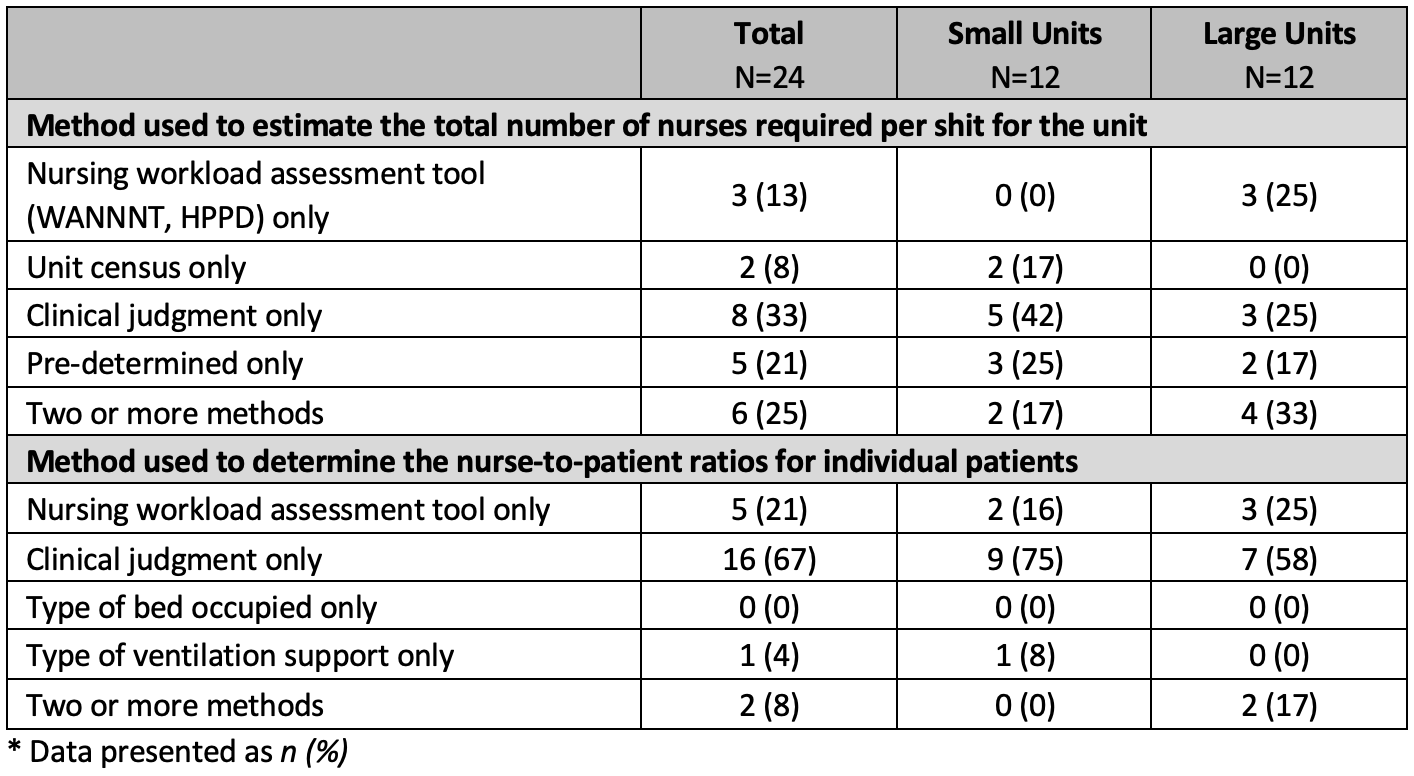
Respondents relied on a variety of methods to estimate the total number of nurses required per shift: 13% used a nursing workload assessment tool, 8% used unit census, 33% used clinical judgment, 21% used pre-determined ratios, and 25% used ≥2 methods (Table 1). In contrast, two-thirds of respondents relied on their clinical judgment to estimate the individual nurse-to-patient ratios.
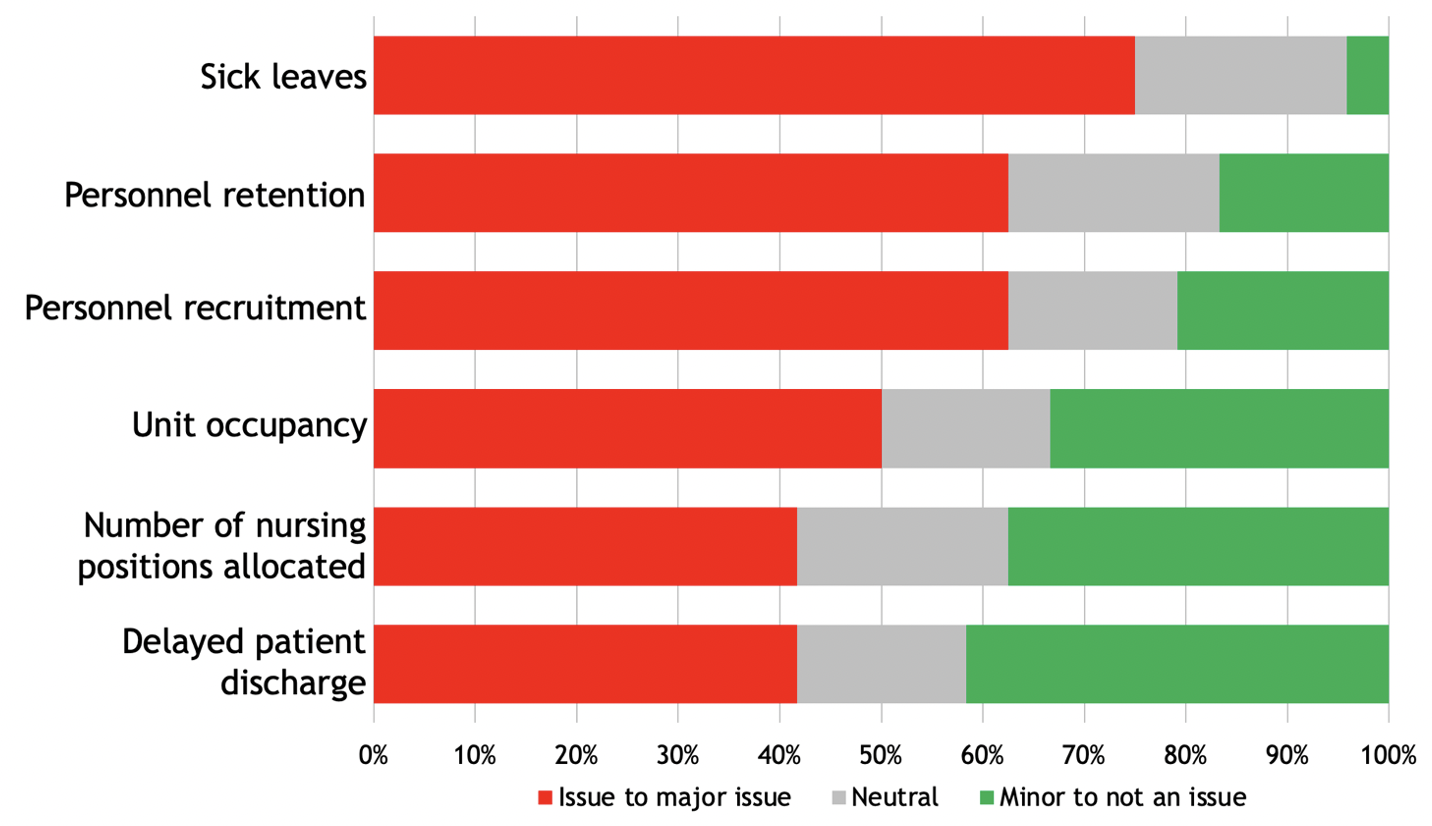
NICUs managers face similar care structure challenges – sick leaves, personnel recruitment and retention, and unit occupancy were reported as being an “issue to major issue” by 75%, 63% and 50%, respectively, of respondents (Figure 1).
Unit’s median reported occupancy was 85% [IQR 80-90] of funded bed capacity. Furthermore, 18/24 (75%) respondents believed that unit occupancy can increase the risk of adverse patient outcomes. Among them, the median occupancy considered to be associated with worst outcome was 90% [IQR 85-95] and the median occupancy at which units start implementing mitigation strategies is 95% [IQR 90-100] (Figure 2). At that point, the most common strategies implemented were to implement additional voluntary nursing resources, accelerate patient transfer and attempt to divert patient admissions.
Conclusion(s): NICU managers across the country shared similar perspectives in terms of staffing and occupancy challenges. This study emphasizes the need for national initiative to inform managers on variables associated with adverse neonatal outcomes and to elaborate mitigation plans.
.png)
