Nephrology: Clinical
Nephrology 3: Dialysis and Diversity and Equity in Kidney Health
279 - Influence of Social Determinants of Health on Patterns of Care for Children with High-Risk Kidney Disease
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 279
Publication Number: 279.252
Publication Number: 279.252
Rebecca R. Scobell, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Fahmida Sarmin, Drexel University College of Medicine, Philadelphia, PA, United States; Alyssa Ciarlante, Children's Hospital of Philadelphia, Havertown, PA, United States; Angela M. Ellison, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Michelle Denburg, Children's Hospital of Philadelphia, Philadelphia, PA, United States
- RS
Rebecca R. Scobell, MD, MSCE (she/her/hers)
Instructor
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Children with chronic kidney disease (CKD) are at risk for acute complications requiring hospitalization and progression to end stage kidney disease (ESKD) requiring dialysis or transplant. Significant disparities in CKD outcomes exist between Americans of different racial, ethnic, and socioeconomic backgrounds. Furthermore, a recent study showed that children who receive “irregular” care have a significantly increased risk of requiring emergent dialysis (versus planned dialysis or pre-emptive transplant) as compared to those receiving “optimal” care. The Childhood Opportunity Index (COI) is a validated composite index comprised of 29 indicators of social determinants of health (SDoH) linked to the US census.
Objective: Describe patterns of health care utilization observed in a cohort of patients with high-risk kidney disease by measurable SDoH.
Design/Methods: We assembled a cohort of patients with high-risk kidney disease, defined as steroid resistant nephrotic syndrome, steroid sensitive nephrotic syndrome on a steroid-sparing medication, lupus nephritis, and/or advanced CKD (eGFR < 30 mL/min/1.73m2, not on dialysis), actively followed at a single pediatric health system 7/1/2019 - 6/30/2022 by leveraging existing reporting workbench and population health management tools. Criteria for inclusion were based on the most recent routine visit. Rates of different types of health care encounters were compared across COI and race/ethnicity categories using Kruskal-Wallis tests. The nonparametric test for trend in rates was performed across COI categories.
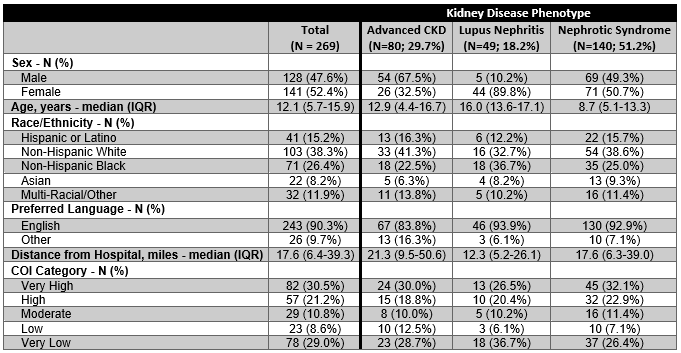
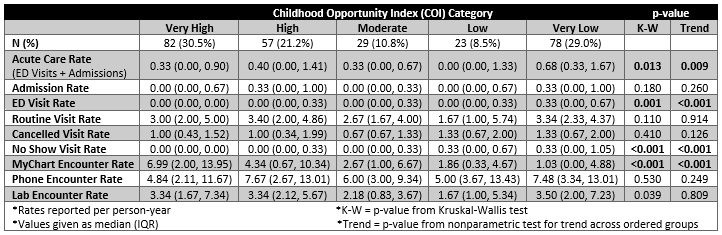
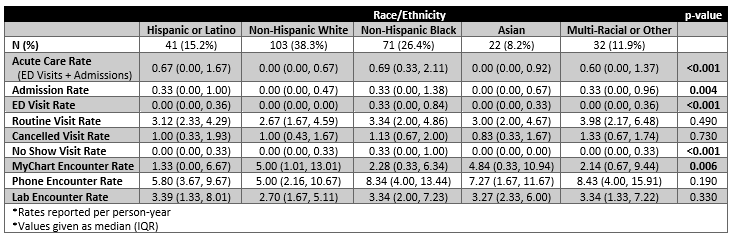
Results: Of the 269 patients in the cohort, 52.4% were female, median age 12.1 (IQR 5.7-15.9) years, and median follow-up time 2.9 (IQR 2.2-2.9) years (Table 1). Differences in rates of acute care visits by COI were driven by emergency department (ED) visits which were increased in children from very low opportunity areas (Table 2) and those of non-Hispanic Black race/ethnicity (Table 3). Rates of “no show” visits were highest for children from low and very low opportunity areas and of non-Hispanic Black race/ethnicity. In contrast, rates of MyChart (electronic patient portal) encounters increased incrementally from very low to very high COI categories and were lowest in patients of Hispanic or Latino ethnicity.
Conclusion(s): Significant differences in rates of ED visits, “no show” visits, and MyChart encounters were observed across COI and race/ethnicity categories. Gaining a better understanding of health care utilization patterns is necessary to design interventions to promote equitable access to optimal care in patients with high-risk kidney disease.