Neonatal-Perinatal Health Care Delivery: Practices and Procedures
Neonatal-Perinatal Health Care Delivery 3: Practices: Growth & Nutrition, Potpourri
763 - Growth and morbidity outcomes in response to a neonatal sodium supplementation protocol
Publication Number: 763.247

Elliot J. Stalter, BA (he/him/his)
Medical Student
University of Iowa Roy J. and Lucille A. Carver College of Medicine
Iowa City, Iowa, United States
Presenting Author(s)
Background:
High obligate urine sodium (Na) losses render preterm infants susceptible to Na depletion, which is associated with impaired somatic growth. An individualized Na supplementation protocol was established at the University of Iowa Neonatal Intensive Care Unit (NICU) in 2016 based upon urine Na concentrations. Use of the protocol results in an average increase in Na intake of 1.5-2 mEq/kg/d between 2-8 weeks of age.
Objective:
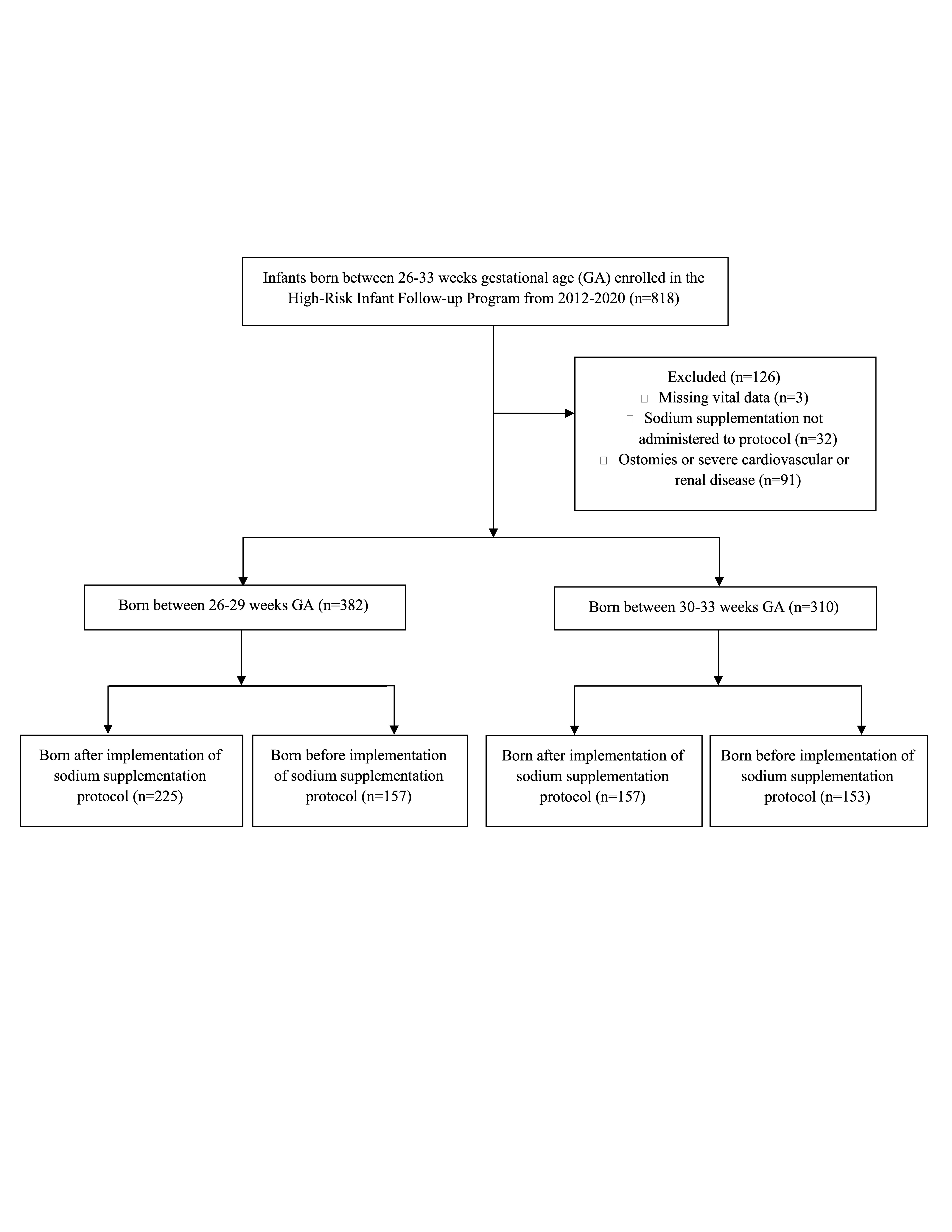
We performed a retrospective cohort study of 692 infants born between 260/7-336/7 weeks gestational age (GA) to compare body weight and head circumference growth trajectories and adverse health outcomes between infants cared for before (2012-15, pre) and after (2016-20, post) implementation of the protocol.
Design/Methods:
Total body weight and head circumference z-scores were obtained for 225 post and 157 pre infants born between 260/7-296/7 weeks GA and 157 post and 153 pre infants born between 300/7-336/7 weeks GA. Growth parameters were examined at birth and 2-, 4-, 6-, 8-, and 16-weeks postnatal age. Within- and between-group changes over time were assessed using repeated measures generalized linear models controlling for GA, sex, and birthweight. Groups were compared on the incidence of hypertension, hypernatremia, necrotizing enterocolitis, bronchopulmonary dysplasia, culture positive sepsis, time on mechanical ventilation, and length of stay.
Results:
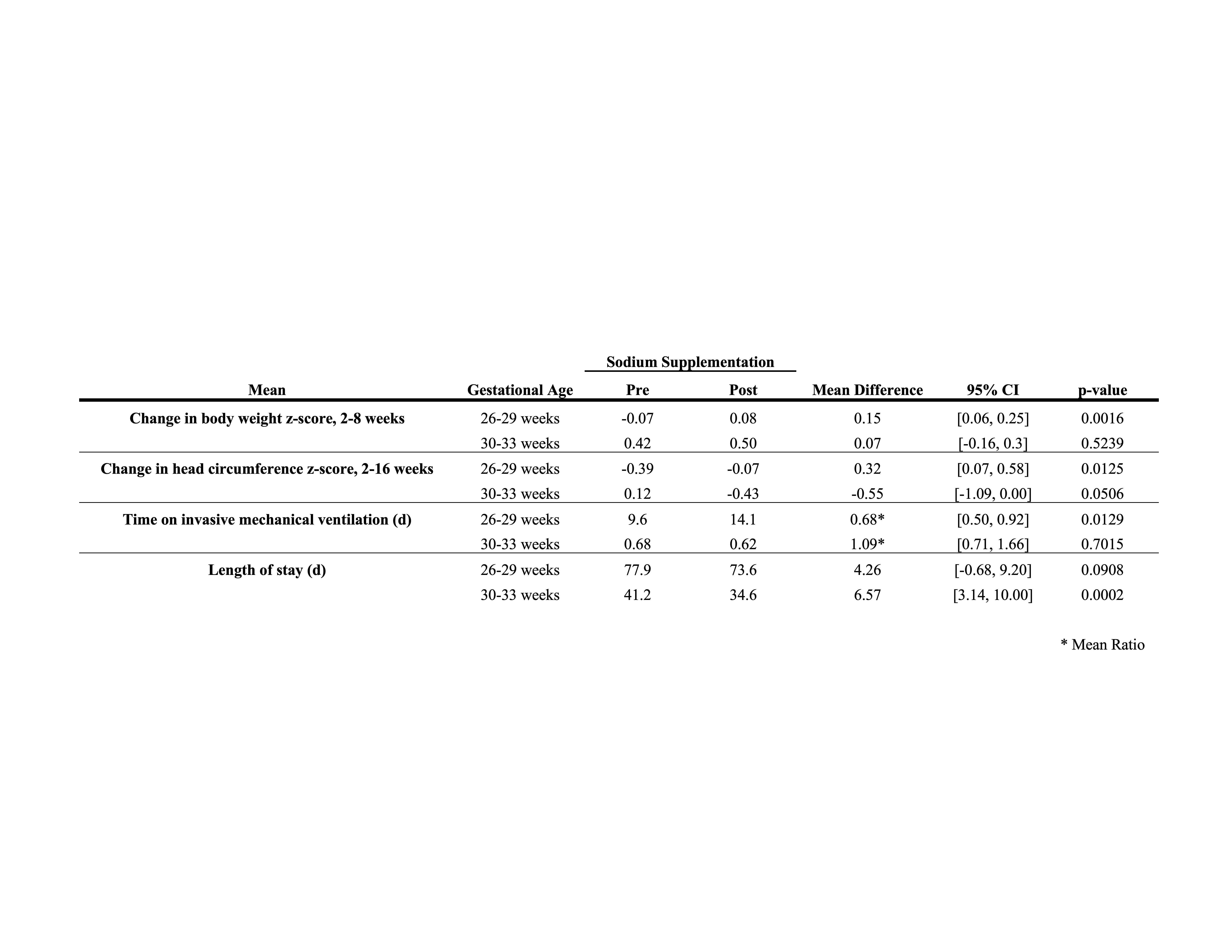
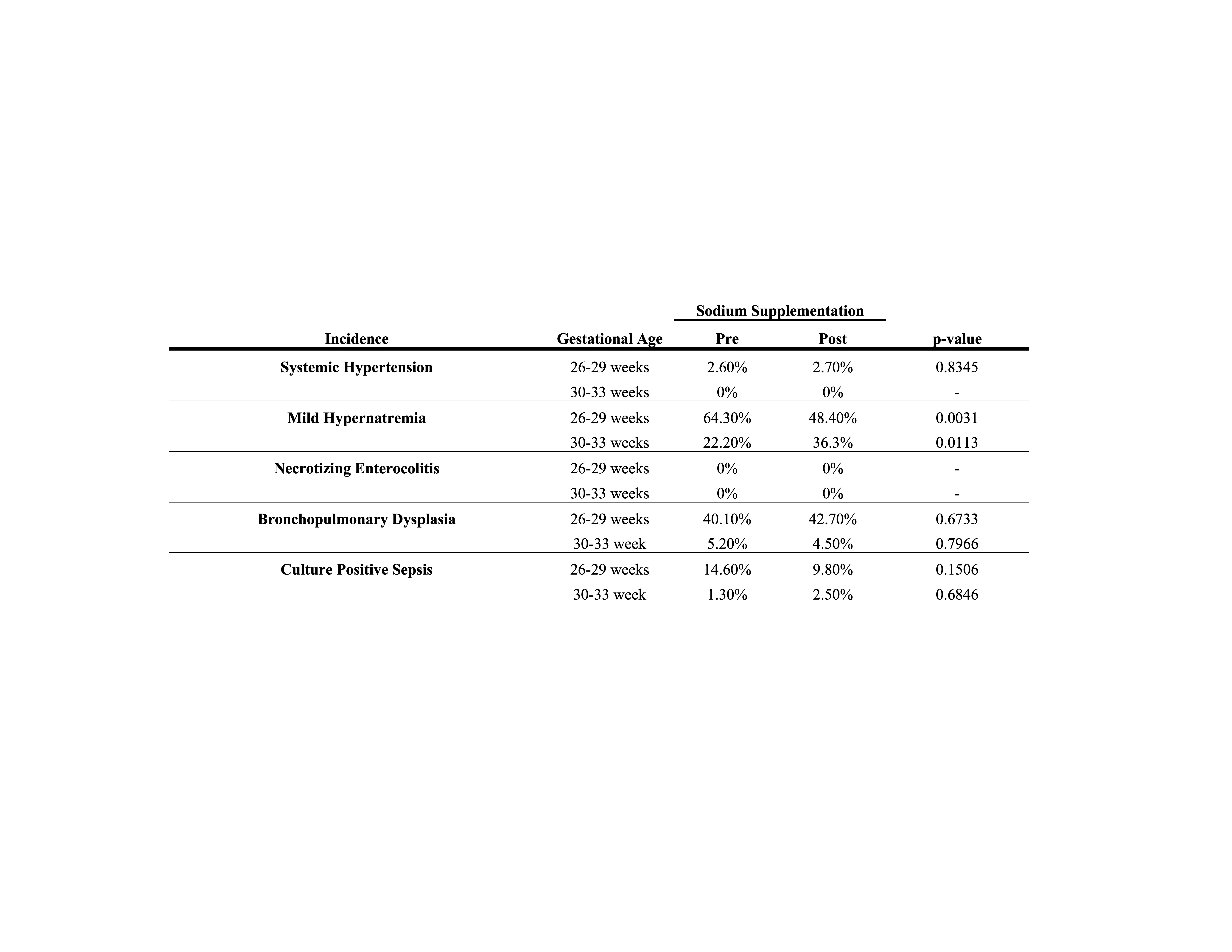
Within the 260/7-296/7 weeks GA cohort, Na supplementation was associated with increased mean body weight z-score at 8-weeks postnatal age (p = 0.0016) and increased mean head circumference z-score at 16-weeks postnatal age (p = 0.0125). Post infants spent fewer days on invasive mechanical ventilation than pre infants (p = 0.0129) and experienced a decreased incidence of mild hypernatremia (146-149 mEq/L; p = 0.0031). Within the 300/7-336/7 weeks GA cohort, no differences in weight or head circumference were identified. Length of stay was greater in the 300/7-336/7 weeks GA post cohort (p = 0.0002). Na protocol use was not associated with systemic hypertension, necrotizing enterocolitis, bronchopulmonary dysplasia, or culture positive sepsis for either GA cohort.
Conclusion(s):
Extremely preterm infants receiving protocol-based Na supplementation demonstrated better early-life weight gain and increased head circumference as well as reduced time on invasive mechanical ventilation and decreased incidence of mild hypernatremia compared to historical controls.