Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 2: Hematology
130 - Thrombin Generation is Enhanced in Platelet-Rich Plasma in Preterm Compared to Full-Term Infants; The EVENT Study
Publication Number: 130.239

Claire A. Murphy, MB, PhD
Specialist Registrar Neonatology
Rotunda Hospital
Dublin, Dublin, Ireland
Presenting Author(s)
Background:
Very preterm infants are at risk of intraventricular haemorrhage, have prolonged standard clotting tests, hypo-reactive platelets in vitro and reduced levels of coagulation factors. Despite these deficiencies, Calibrated Automated Thrombography (CAT), a global coagulation assay, has been used to demonstrate similar or enhanced thrombin generation in preterm compared with term infants in platelet poor plasma (PPP). However, the effect of platelets on thrombin generation in the premature infant has not been described.
Objective:
We aimed to characterize phospholipid-dependent thrombin generation in platelet-rich (PRP) and platelet-poor plasma (PPP) in premature infants in both umbilical cord blood (UCB) & peripheral neonatal blood (PB) using CAT.
Design/Methods:
In this prospective observational study, PRP and PPP were prepared by centrifugation from citrated UCB and PB collected from premature infants (24 - 31 weeks) and healthy term controls ( >37 weeks). Thrombin generation in PRP was assessed by CAT using PRP reagent (contains tissue factor only (1pM)). The experiment was repeated in a subset of infants in PPP using PRP reagent. This assay is dependent on the phospholipid content of PRP/PPP (platelets/ extracellular vesicles (EVs)). Ethical approval and parental consent was obtained.
Results:
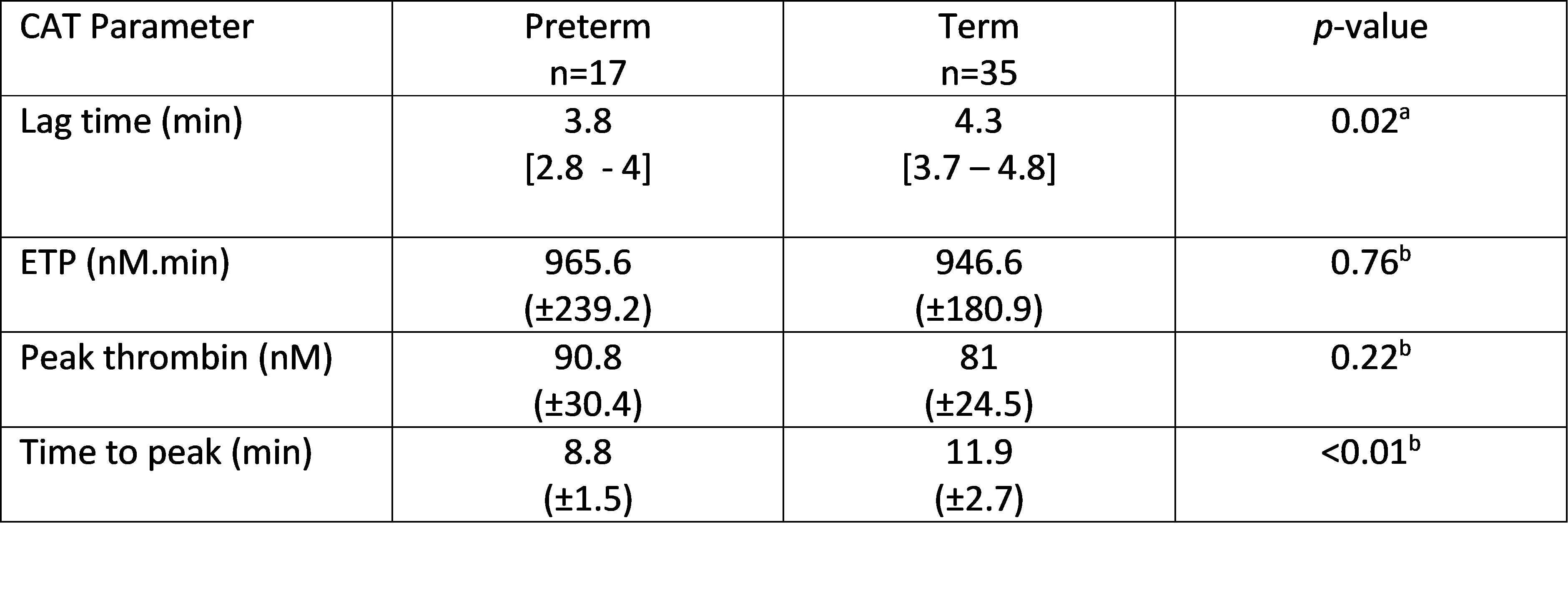
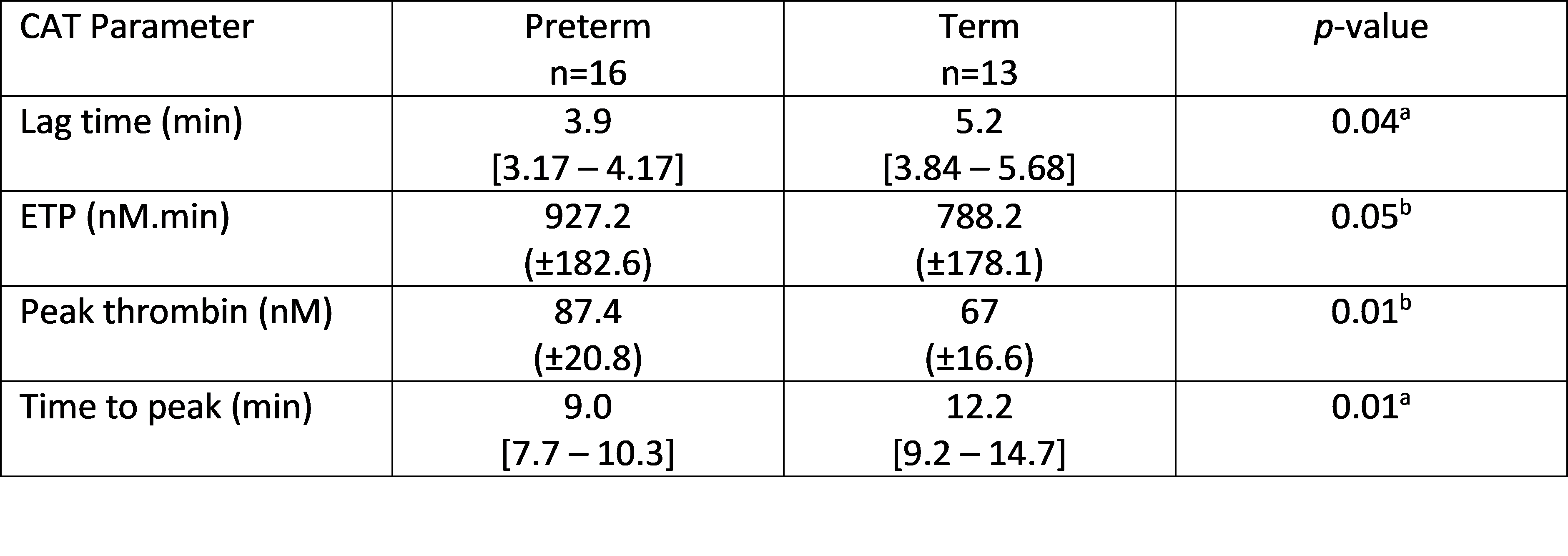
In UCB PRP, thrombin generation was accelerated in the preterm group, demonstrated by a reduction in lag time (LT) and time to peak thrombin (TTP) (Table 1). In PB PRP, thrombin generation was also enhanced in preterm infants, demonstrated by a shortened LT and TTP, and an increase in peak thrombin and endogenous thrombin potential (ETP) (Table 2).
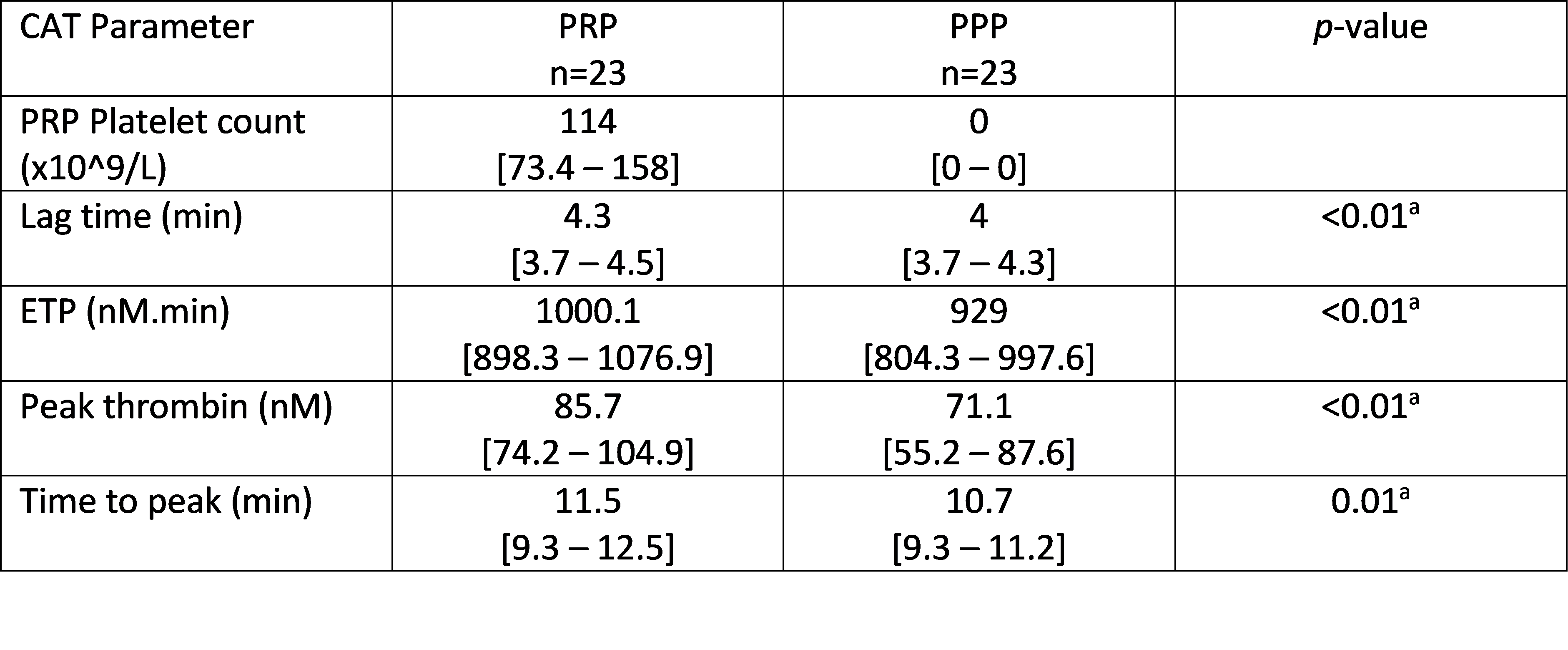
In a subset of infants (n=23 term, n=10 preterm), CAT was assessed in paired PPP and PRP from UCB using PRP reagent, to evaluate the effect of platelets. The presence of platelets caused a small increase in the ETP and peak thrombin in preterm and term infants. However, the presence of platelets caused a prolongation in the LT and TTP in the term group only (Table 3).
Conclusion(s):
Thrombin generation in PRP is enhanced in preterm infants in UCB and PB. In spite of reported “hypo-reactive” preterm platelets, it appears they adequately support thrombin generation.
Interestingly, the presence of platelets in term infants prolonged the initiation of coagulation. This was unexpected and not observed in preterm infants. This warrants further study in view of the PlaNeT-2 Study findings, where the liberal transfusion of adult platelets to thrombocytopenic preterm infants resulted in an increased risk of haemorrhage, possibly due to a developmental platelet mismatch.