Emergency Medicine: All Areas
Emergency Medicine 7
371 - Describing and Categorizing Patients Identified by Automated IPSO (Improving Pediatric Sepsis Outcomes) Criteria who do not have Sepsis
Publication Number: 371.211

Savannah Brackman, MD (she/her/hers)
Resident Physician
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background:
The Improving Pediatric Sepsis Outcomes (IPSO) criteria were developed to facilitate identification of sepsis cases in the Electronic Health Record (EHR) for quality improvement. These criteria have been used to identify cases in which sepsis diagnosis and treatment were initiated, an important population for process-based QI regardless of final diagnosis. Prior investigators have identified a limitation of these criteria for epidemiology and research: they include patients receiving early antibiotic and fluid treatment who do not ultimately have a sepsis diagnosis. The proportion of IPSO Sepsis patients who do not have sepsis and their non-sepsis diagnoses have not been systematically described.
Objective:
1) Describe the proportion of pediatric patients identified via IPSO sepsis criteria who do not have sepsis; 2) Determine the non-sepsis diagnoses that meet IPSO criteria.
Design/Methods:
Pediatric patients (age 31 days – 18 years) presenting to 26 emergency departments sharing a single EHR from 2015-2021 were identified using IPSO sepsis criteria. Inclusion criteria were IPSO-defined sepsis [Table 1] and admission to the hospital of one of the included EDs or to the regional children’s hospitals. Acute appendicitis and transfers outside of included hospital system were excluded.
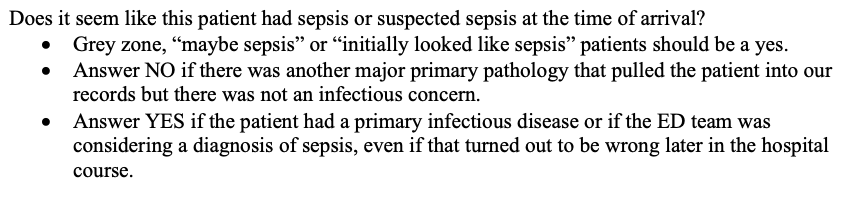
Chart review was conducted to determine ground-truth diagnoses. We defined non-sepsis as an alternate, non-infectious primary pathology [Table 2]. Three physician reviewers independently reviewed 10 charts and classifications were compared, first yielding a Cohen’s kappa of 0.74. Discrepancies were discussed and reconciled and classifications clarified. Subsequently, 10 different charts were independently reviewed by the three physicians and classifications compared, yielding perfect agreement (kappa 1.0). Cases that were classified as having non-sepsis diagnoses were compiled and categorized.
Results:
We identified 633 cases of IPSO-defined sepsis, of which 58 (9.2%) cases were classified as non-sepsis (Table 3). Median age of non-sepsis diagnoses was 10.5 years old [IQR 4-17]. The most common non-sepsis diagnoses were trauma, toxic ingestions, and non-infectious gastrointestinal diagnoses.
Conclusion(s):
This study systematically describes the proportion of cases identified by IPSO criteria that were not cases sepsis and the most common alternative diagnoses. These diagnoses could be used to further refine IPSO sepsis criteria for quality improvement efforts. Our main limitation is that results may not generalize to other health systems based on local disease patterns (e.g., trauma or substance use patterns).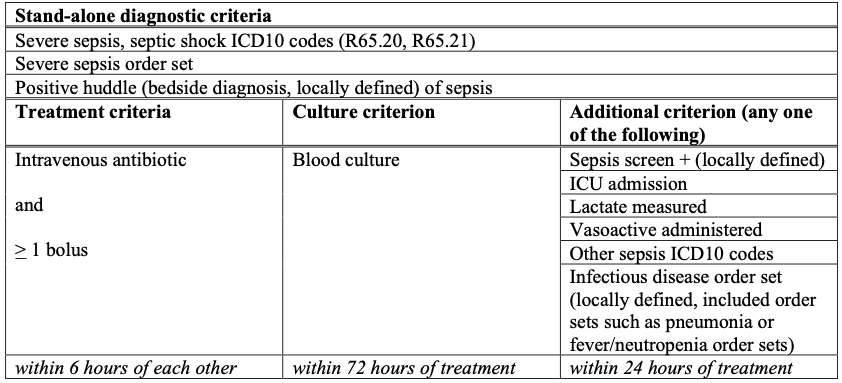
.png)
